Until recently, the role of ectopic fat deposits in obese pancreatic areas, as well as its impact on the development of type 2 diabetes mellitus, remained poorly understood.
Intermittent fasting has been previously reported to improve glucose homeostasis, insulin sensitivity, and prevent fatty liver disease. However, the effect of intermittent fasting on the processes of lipogenesis in the pancreas and the functional activity of β-cells remained uncertain.
Read the article on estet-portal.com about a clinical study on the effectiveness of intermittent fasting as a prevention of diabetes.
- Impaired lipid metabolism in diabetes mellitus
- Impact of intermittent fasting on lipid metabolism
- Intermittent Fasting Study Results
- Intermittent fasting modes
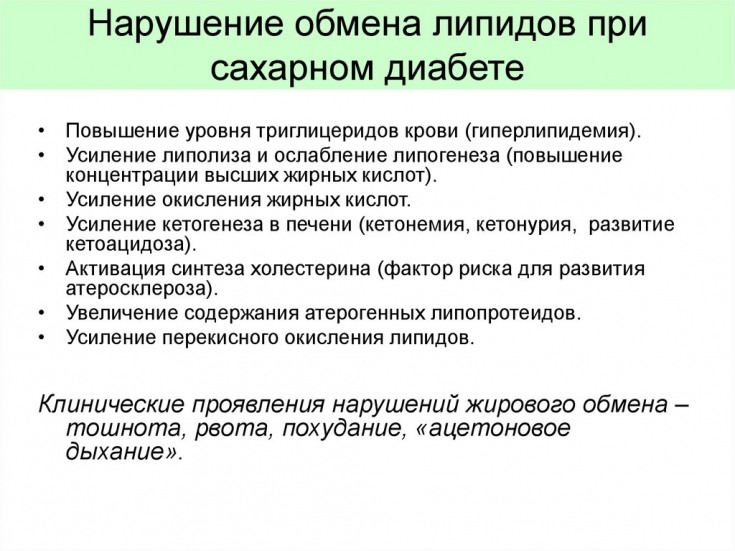
Impaired lipid metabolism in diabetes mellitus
In a new experimental study by scientists from the German Center for Diabetes Research, it was found that laboratory animals genetically predisposed to the development of diabetes mellitus have more pronounced processes of fatty infiltration of pancreatic tissues.
Follow us on Instagram!
Along with this, intermittent fasting prevents the development of both fatty infiltration and type 2 diabetes. In addition, it has been proven that adipocytes derived from the pancreas are able to change the endocrine properties of the pancreas in relation to to insulin.
Impact of intermittent fasting on lipid metabolism
The aim of the work was to evaluate the effect of intermittent fasting on the processes of lipogenesis in the pancreas, as well as its effect on the functional activity of the islets of Langerhans. During the experimental study, laboratory animals with simulated obesity received a diet with a high fat content (main observation group) or were kept on intermittent fasting every other day (comparison group).
Diabetic acidosis – life-threatening complication of diabetes
In animals of these groups, as well as in the control group of mice, the feeding regimen of which was unlimited, the volumes of accumulation of adipose tissue in the structures of the pancreas, glucose homeostasis, insulin sensitivity and the functionality of the islets of Langerhans were determined. The observation period lasted 5 weeks. Thus, it was found that among obese animals that were on the intermittent fasting regimen, the most optimal profile of blood glucose regulation was observed along with the least pronounced accumulation of fat both in the structures of the pancreas (32%) and in the tissues of the liver (35% ) against animals of the main group.
Therapeutic Strategies for the Development of Insulin Analogs
But in animals of the control group, which were fed without restrictions, manifestations of insulin resistance, unexpressed infiltration of adipose tissue in the pancreas and, at the same time, activation of processes of fatty infiltration in the liver were observed. Simultaneously, model obesity animals fed a high-fat diet showed increased accumulation of fat in each organ along with a decrease in pancreatic insular activity.

Further experiments with co-cultivation of β-cells and fat cells showed that pancreatic adipocytes are able to actively induce insulin hypersecretion and releasing free fatty acids compared to the functional orientation of white adipose tissue adipocytes.
In this regard, the authors noted that the accumulation of adipose tissue in the pancreas and hypersecretion of insulin by β-cells, followed by their functional depletion, are interconnected by links of a single pathological process, which may be a precursor to the development of diabetes mellitus.
Intermittent Fasting Study Results
Based on this evidence, the researchers concluded that pancreatic adipocytes play an important role in the metabolic changes that occur in the development of diabetes mellitus. However, convincing evidence has been obtained that the manifestations of the identified pathological changes can be corrected by observing a diet based on intermittent fasting.
Medicinal nutrition for diabetic nephropathy
Thus, the presented data emphasize that in preventing the development of diabetes mellitus, not only inhibition of fatty liver processes is important. The method of intermittent fasting, according to scientists, may indeed be a promising therapeutic approach in the future. The advantages of the method are undeniable: non-invasiveness, easy and physiological integration into everyday life, as well as the absence of the need for additional pharmacotherapy.
Intermittent Fasting Modes
Extrapolating the intermittent fasting technique to clinical practice and the daily lives of patients with diabetes, the authors noted that intermittent fasting involves abstaining from eating for certain time intervals. At the same time, it is allowed to drink water, unsweetened tea and black coffee around the clock. Depending on the method, such fasting can last from 16 to 24 hours, or alternatively, for two days a week, a person consumes no more than 500-600 kcal.
New treatment for diabetic foot
The most well-known variant of intermittent fasting is the 16:8 method, which involves eating only an 8-hour interval during the day and fasting for the next 16 hours. In this case, one meal, usually breakfast, is canceled. Therefore, it would be appropriate to inform that for an adult, the primary physiological biorhythmic interval between meals (day) and rest (night) is considered to be a period of at least 12 hours.
The hormone melatonin may increase the risk of diabetes









Add a comment