Chronic pelvic pain (CP) ─ is moderate to severe pain in the lower abdomen that has lasted at least 3-6 months. Pain provokes functional disorders, negatively affects personal relationships, mood, intimate life and worsens the general health of a woman. In terms of prevalence, CPP is not inferior to bronchial asthma or back pain. It is a common cause of disability and reduced productivity, which in turn significantly increases healthcare costs.
Find out in the article on estet-portal.com how to determine the cause of chronic pelvic pain syndromeand what approaches to treat this pathology.
- diagnosis of chronic pelvic pain syndrome
- Laboratory and clinical research in chronic pelvic pain
- drug therapy for chronic pelvic pain syndrome
Chronic Pelvic Pain Syndrome Diagnosis
To establish a diagnosis, it is extremely important to carefully collect a medical and surgical history, to clarify in detail the features and characteristics of pain.
Follow us on Instagram!
Gynecological status requires special attention, including the course of pregnancy and childbirth, the presence of dyspareunia or injuries. A detailed systemic survey should focus on the reproductive, digestive, musculoskeletal, urinary and neuropsychic systems, which will help identify possible disorders and determine the direction of further diagnostic search.
How should a disorder of the genitourinary microbiome be treated?
It is necessary to conduct a purposeful detailed objective examination. The review is determined by the characteristics of the anamnesis, but necessarily requires a detailed examination of the abdomen and pelvis, which should be carried out slowly and carefully, assessing areas of increased sensitivity, discomfort or tenderness, the presence of masses or other pathological changes.

The pelvic examination begins with a visual examination to look for redness, discharge, sores, lesions, cracks, abrasions, peeling, and other abnormalities. A moistened cotton swab may be used to assess local tenderness at the vulva or vaginal opening.
The manual part of the pelvic exam is started with one finger, noting any soreness, discomfort, or spasm.
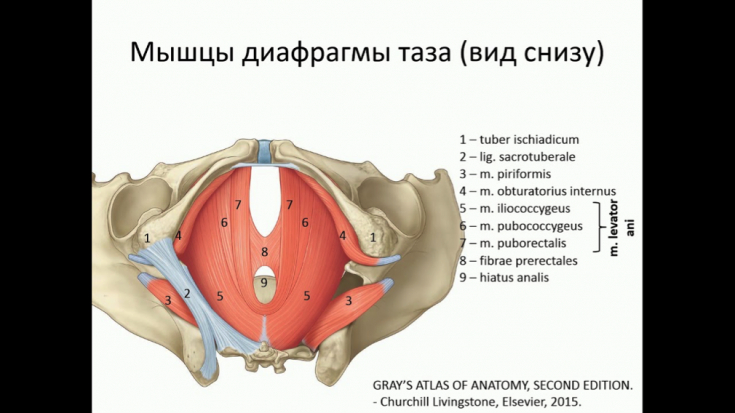
The next step is to palpate the muscles of the anus to assess tone and tenderness. Next, other parts of the pelvic floor are examined, paying attention to the sensitivity or soreness of the bladder and musculoskeletal structures. Complete the review with a bimanual examination that allows assessment of the size and mobility of the uterus, revealing tenderness or nodes.
Laboratory and clinical research in chronic pelvic pain
Given the broad differential diagnosis of chronic pelvic pain syndrome, further diagnostic search is based on the results of the history and physical examination. Comprehensive laboratory testing is of limited value in determining the cause of the pathology. If bladder symptoms are present, particularly if cystitis is suspected, a urinalysis is done.
Acute cystitis: a common female problem
identified by palpation. However, the routine use of imaging techniques is not recommended. If pelvic stasis syndrome is suspected, USG may be considered to assess the need for other imaging modalities ─ CT or
drugs that are commonly prescribed for the treatment of chronic pain can be prescribed. Tricyclic antidepressants (amitriptyline, imipramine) reduce pain and depressive symptoms and improve sleep.
Modern views on the treatment of asymptomatic bacteriuria
A small randomized controlled trial (RCT) suggests that gabapentin is more effective than amitriptyline in reducing symptoms of chronic pelvic pain. Current guidelines consider amitriptyline and gabapentin as first-line therapy, while nortriptyline and pregabalin are alternatives. Although specific studies are not yet available,
venlafaxine and duloxetinecan be used to control chronic pelvic pain. The latter is indicated for women who have CPP combined with depression and stress urinary incontinence. Evidence for the use of nerve blocks and neuromodulation to control chronic pelvic pain is rather weak. Therefore, they can only be used as one of the components of complex treatment provided that it is carried out by a highly qualified specialist.
More useful information on our YouTube
-channel:









Add a comment