Erythema, burning and pain, itching, peeling – possible signs of hypersensitivity of the skin, which may occur in response to irritating factors. Could such a reaction or its intensity be associated with the presence of excess weight in patients? In the article estet-portal.com, Drs. Yana Yanovskaya and Lana Kasparane talk about the role of obesity and metabolic syndrome in violation of the barrier function of the skin, which can lead to a number of dermatological diseases and skin hypersensitivity.
- Metabolic syndrome: criteria and clinical skin manifestations
- Why does skin hypersensitivity occur
- Barrier function, inflammation and skin sensitivity
- Oxidative stress, metabolic syndrome and skin sensitivity
- The effect of endocrine disorders in MS on skin sensitivity
Metabolic Syndrome: Criteria and Clinical Skin Manifestations
Metabolic Syndrome (MS) – a disease in which the patient is centrally obese (female > 80 cm, male > 94 cm) and meets at least two of the following criteria:
- elevated triglycerides or blood glucose;
- low high-density lipoprotein;
- high blood pressure.
Various clinical skin manifestations associated with the metabolic syndrome and/or its components have been identified in several international studies.
Follow us on Facebook!
The list of diseases includes:
- psoriasis;
- androgenetic alopecia;
- acanthokeratoderma;
- soft fibromas;
- Wilson's lichen;
- acne inversion;
- systemic lupus erythematosus;
- and even skin cancer.
As is known, in metabolic syndrome, the amount of inflammatory cytokines is increased and a chronic inflammatory reaction in the skin is observed. Therefore, the connection of MS with hypersensitivity of the skin, which is accompanied by activation of immune cells.
Why does skin hypersensitivity occur
Skin sensitivity manifests itself with varying degrees of intensity, determined by subjective indicators, such as burning and pain, in response to irritating factors (wind, high temperature, dryness, stress, hormonal imbalance, improper care behind the skin).
Read also: Why the skin reaction to irritation is inadequate
The pathophysiology of skin hypersensitivity is not fully understood. There are several theories to explain skin hypersensitivity, such as:
- changes in the skin barrier;
- activation of keratinocytes;
- neurogenic inflammation/neural mechanism;
- reduced skin tolerance;
- genetic predisposition.
Even in the absence of documented clinical signs of skin hypersensitivity, the subjective symptoms of patients, especially those with metabolic syndrome, cannot be ignored.
The most frequently considered potential mechanisms:
- change in skin barrier function;
- neurogenic inflammation.
Barrier function of the stratum corneum of the epidermis leaves cells of the immune system and sensory nerves vulnerable, resulting in a pronounced response to otherwise harmless stimuli.
Barrier function, inflammation and skin sensitivity
One of the functions of the skin – protection of the body from negative environmental factors at three levels:
- physical (protection against mechanical damage, uncontrolled loss of water and substances dissolved in it) – stratum corneum, nuclear cells of the epidermis and desmosomes;
- chemical/biochemical – internal immunity (fats, organic acids, lysosomes and antimicrobial peptides);
- humoral and cellular immune system (lymphocytes, neutrophils, monocytes and Langerhans cells).
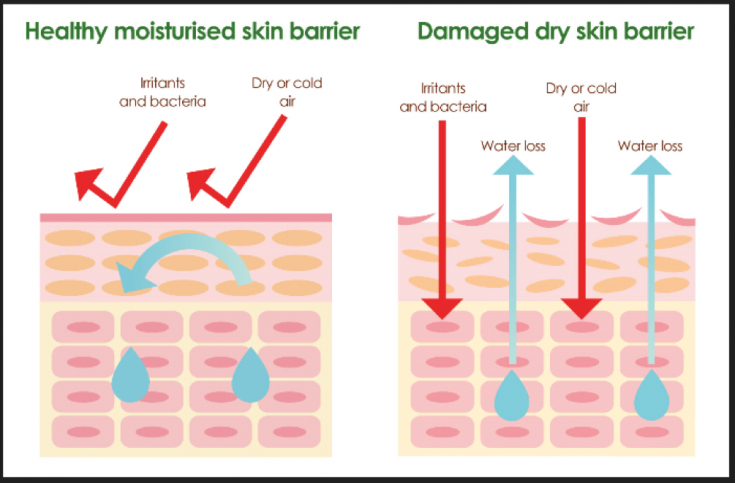
It has been established that in people with morbid obesity, the restoration of the skin barrier is impaired. The skin barrier is formed by differentiation of keratinocytes and constant regeneration. During differentiation, keratinocytes go through different stages of development. This is a complex process involving proteins, fatty acids, fats and enzymes. Their functions and expression are controlled by cytokines and extracellular signaling molecules and receptors. Therefore, in order to ensure the proper development of the epidermal barrier, the correct regulation of all components involved in the differentiation process, as well as their timely and sufficient expression, is necessary.
Different cytokines act at different levels to control the formation of the skin barrier. Therefore in case of cytokine expression dysregulation:
- transepidermal water loss increases;
- the function of the epidermal barrier is reduced;
- Inflammatory reaction intensifies.
In response to minimal external stimulation, IL-1α, IL-1β; and TNF-.alpha. Small amounts of IL-6 are found in the cells of the epidermis. However, in the event of a violation of the skin barrier, their number rapidly increases. These cytokines play a role in the formation and repair of the epidermal barrier.
You may also be interested in: Skin barrier function in atopic dermatitis
In the skin of patients with metabolic syndrome, there are more inflammatory cytokines (TNF-α, IL-6, MCP-1), angiotensin and other adipocytokines produced by fat cells, which are part of the innate immune system, regulating inflammation. Dysregulation or secretion of these adipokines caused by adipose tissue dysfunction may be a factor in the development of complications associated with obesity. At the same time, these cytokines can stimulate epidermal proliferation and rejuvenation. However, in chronically elevated levels of inflammatory cytokines, as in the case of MS, the inflammatory cascade can lead to systemic activation of the immune system.
Oxidative stress, metabolic syndrome and skin sensitivity
Oxidative stress is assigned a central role in the pathogenesis of the metabolic syndrome. The skin plays an important role in the metabolism and excretion of xenobiotics, endogenous bioactive substances, fats and cholesterol.
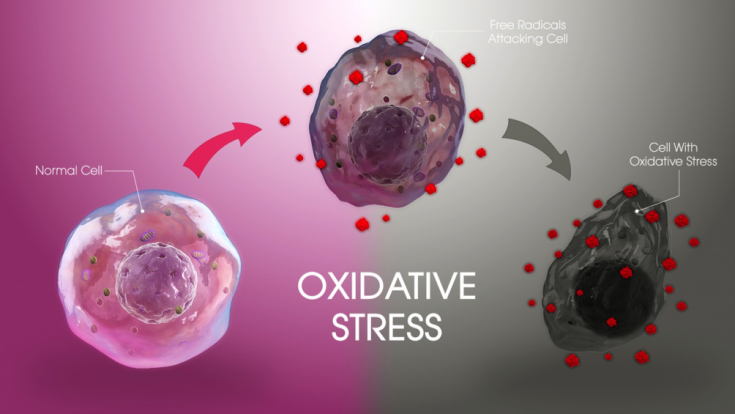
Xenobiotics such as exogenous chemicals, drugs, pollutants, cosmetics and food ingredients – the main sources of reactive oxygen species, which are believed to be part of the pathogenesis of a number of skin diseases.
Inflammation is well known to be one of oxidative stress, and pathways that lead to the production of inflammatory mediators such as interleukins are associated with oxidative stress.
The various components of the metabolic syndrome are subject to seasonal variations: blood pressure and blood cholesterol levels rise in winter.
Being more sensitive to ambient temperature than other organs, the skin may be partly responsible for the association between fluctuations in blood pressure and ambient temperature.
Most patients with sensitive skin report unpleasant sensory reactions to cold temperatures and humidity, resulting in a decrease in moisture levels in the stratum corneum. More often such conditions occur in winter. Therefore, seasonal variations in MS are more pronounced in patients with sensitive skin.
Influence of endocrine disorders in MS on skin sensitivity
Adipocytes secrete several endocrine peptides such as leptin and adiponectin. These substances are involved in acute and chronic inflammatory processes through the regulation of cytokine expression, modulating the balance of type 1 and type 2 helper T cells, as well as changes in glucose metabolism and vascular endothelial biology.

Most obese patients have elevated circulating leptin in conditions of functional leptin resistance. Leptin receptors are found in tissues, incl. keratinocytes, fibroblasts, endothelial cells and adipose tissue. Leptin also plays a role in the formation of the epidermal barrier, promotes wound healing, stimulates:
- fibroblast proliferation;
- collagen synthesis;
- endothelial cell growth;
- angiogenesis.
However, elevated levels of leptin in patients with MS are vascular toxic and lead to capillary leakage and formation of avascular zones.
In clinical cases persistent or transient erythema and telangiectasia have been observed in the majority of patients with sensitive skin. Therefore, with increased sensitivity of the skin and MS, these clinical signs are more pronounced.
Adiponectin plays a role in the production of sebum, contributing to the formation of differentiated structures of the sebaceous glands and an increase in their number.
Sebocyte lipids are known to be secreted to the surface of the skin, where they perform important barrier functions.
Read also: Working with sensitive, reactive skin prone to couperose and rosacea: the choice of drugs
But in patients with metabolic syndrome, ur adiponectin level is reduced. In addition, its level is inversely proportional to the number of MS criteria – as the number of criteria increases, the level of adiponectin decreases, as does the barrier function, and the sensitivity of the skin increases accordingly.
Sensitive skin affected by metabolic syndrome is characterized by more pronounced
:
skin barrier dysfunction;
- inflammation;
- immune reactions;
- oxidative stress;
- seasonal variations;
- reduced ability to regenerate. However, information on the association of hypersensitivity of the skin and metabolic diseases such as obesity, diabetes, and metabolic syndrome is lacking. It is not entirely clear whether metabolic syndrome causes skin sensitivity or vice versa. Further research is needed to answer this question.
According to Prime magazine.
Subscribe to our
YouTube-channel!









Add a comment