Despite the proven relationship between obesity and many chronic diseases, conflicting information is accumulating around the world about the impact of weight on life expectancy. A new obesity assessment paradigm has been introduced by the American Endocrinology Association. Experts believe that many additional factors must be taken into account when assessing the impact of body weight on a patient's health.
How dangerous obesity is for health
In 1950, obesity was included in the international classification of diseases of the World Health Organization (WHO), the main diagnostic criterion for which was the body mass index (BMI). According to the 2004 WHO classification, a BMI in the range of 18.5 to 24.9 kg/m2 is considered normal, a BMI below 18.5 kg/m2 is considered underweight ; with excess weight — BMI 25.00–29.99 kg/m2; A BMI of 30–40 kg/m2 indicates obesity, and more than 40 kg/m2 suggests morbid (morbid) obesity.
Given the prevalence of obesity in the modern world, the term "globesity" appeared in medical articles, emphasizing the significance and globality of this phenomenon. According to the WHO, in 2008 over 1.6 billion adults on the planet were overweight, including more than 500 million — obesity.
Over several decades, the results of a significant number of epidemiological studies have shown the relationship of obesity with arterial hypertension, coronary heart disease (CHD), heart failure, type 2 diabetes mellitus (DM), cancer, bronchial asthma, diseases of the musculoskeletal system. locomotor system, polycystic ovaries, Pickwick's syndrome, obstructive sleep apnea, depression and bulimia.
A number of studies have shown that obesity contributes to a deterioration in the quality of life, the emergence of social, psychological and economic problems, and increases the cost of medical care.
How BMI is calculated and what is the norm
Concurrent prospective studies evaluating the impact of overBMI and obesity on mortality rates have found mixed results. Thus, in a number of studies, mortality rates were correlated not only with the level of BMI, but also with the ethnic features of the structure of different population target groups. So, in 1999 E. Calle et al. published the results of a study that involved more than 1 million people in the United States.
The study showed that long-term mortality rates are minimal at a BMI of 22–26 kg/m2 (with slight variation in subgroups — smokers, non-smokers, men, women, presence or absence of chronic diseases ), in all considered subgroups, mortality was higher with a BMI less than and more than the indicated values. In another study, the lowest mortality rates were reported for African Americans with a BMI of 27 kg/m2 and for White Americans — BMI 24–25 kg/m2. In the "Asian" population, the minimum mortality rates were recorded at a BMI of 22.5-27.5 kg / m2.
Thus, the ideal point value of BMI in the prognostic plan has not been identified, and there is a possibility of an "individual normal" BMI.
What does the "obesity paradox" mean
Furthermore, a number of studies have shown a disturbing pattern of "obesity — risk of chronic disease — risk of premature death", and the term "obesity paradox" has become widely used. It has been shown that among certain population groups (the elderly, patients with chronic renal failure (CRF) and those on hemodialysis, with heart failure), survival is higher among patients who are overweight and obese.
Thus, despite the fact that obesity is associated with an increased risk of developing atrial fibrillation, the AFFIRM (Atrial Fibrillation Follow-up Investigation of Rhythm Management) study found that overall mortality and mortality from cardiovascular disease was lower among patients with overweight and obese than among patients with normal body weight. In 2012, MR Carnethon et al. publish the results of a meta-analysis of 5 large prospective studies in which it was found that among patients in whom diabetes mellitus developed against the background of a normal BMI, mortality from total, cardiovascular and other causes is higher than among patients who developed diabetes mellitus against the background of overweight or obesity. Similar data were obtained in a Korean study (more than 16 thousand people over 20 years old).<
Another major study was done in Taiwan: CH Tseng et al. after adjusting for other factors influencing mortality, they found an inverse relationship between BMI and all-cause mortality.Given the inconsistency of research results and trying to understand the causes of the "obesity paradox", various hypotheses have been put forward to explain this phenomenon. It has been shown that not any, namely abdominal obesity (waist circumference > 88 cm in women and > 102 cm in men), aggravated by smoking, increases the risk of cardiovascular events by 5.5 times. However, in different regions of the world among the population of different population ethnic groups, this index varies significantly and the results of studies do not currently reflect these features.
So far, there is no convincing data in the world explaining the causes of the "obesity paradox". Many experts believe that the data on the “obesity paradox” obtained in studies and meta-analyses are due to methodological research errors (random, systematic, publication errors). As it became clear that BMI is a dubious characteristic of obesity and a highly controversial risk factor, a slightly different approach to the assessment of obesity was formulated: excess BMI in combination with metabolic syndrome is a risk factor.
Other researchers, accepting the existence of the "obesity paradox" as a real fact, are trying to understand the causes of the paradox, realizing that obesity itself is unlikely to be a factor in better survival. Research results suggest that BMI is not a true indicator of the anatomical mass of adipose tissue in the body and does not allow differentiating the ratio of adipose, muscle and bone tissue.
In this regard, to diagnose obesity and evaluate the effectiveness of its treatment, it is proposed to use a number of additional laboratory, instrumental and physical methods for diagnosing the volume of adipose tissue and "metabolically normal" obesity (metabolically healthy obese). The latter include a combination of the following features: BMI over 25, normal levels of cholesterol, blood pressure and blood glucose, maintaining insulin sensitivity, waist circumference in men less than 100 cm, in women — 90 cm, in good physical condition (permanent fitness).
It is interesting that despite the fairly numerous publications on the "obesity paradox", the recommendations of the European Society of Cardiology, even the latter continue to indicate that the minimum rates of cardiovascular mortality are observed with a BMI of 20 to 25 kg / m2. At the same time, these recommendations already contain information about the need to study the relationship between the volume of adipose tissue, determined using magnetic resonance or computed tomography, with long-term clinical outcomes, and to assess changes in the volume of adipose tissue over time.
Thus, today there is no doubt that obesity contributes to the development of a number of chronic non-communicable diseases, and BMI is a simple, reliable screening criterion for assessing normal, overweight and obesity. At the same time, despite a significant number of prospective cohort studies conducted over the past 10-15 years in different countries of the world, it has not been proven that a BMI of 25-35 kg / m2, without taking into account the ethnic characteristics of the constitution, metabolic changes, waist size, fat ratio and muscle tissue, is a risk factor for higher mortality (compared to "normal" BMI).
A new algorithm for diagnosing and assessing obesity
A number of studies have found that people with excess BMI, compared with normal or reduced BMI, have a better survival rate in the presence of a number of chronic diseases (including coronary artery disease). It is these factors that led to the fact that at the 23rd annual scientific congress in 2014, the American Association of Endocrinologists considered a new algorithm for diagnosing obesity, which includes two components:
- evaluation of BMI with correction for ethnic characteristics to identify individuals with an increased amount of adipose tissue;
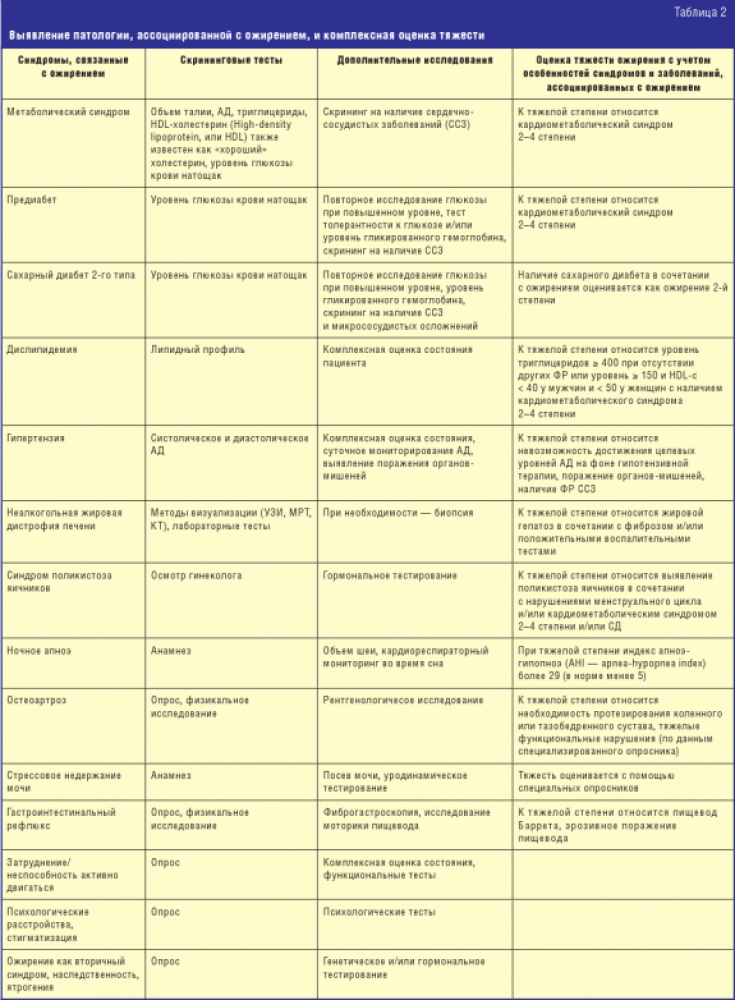
- Presence and severity of complications associated with obesity (Table 1)

2 it is recommended to undergo a medical examination with measurement of blood pressure, waist circumference, fasting glucose, lipid profile, electrolytes, creatinine, liver transaminases.
Consensus members agreed that obesity is a disease, but found it inappropriate to use a number-based approach. According to the participants, the definition of obesity should be based on a comprehensive consideration of the reasons for the increase in the incidence of obesity, on the pathophysiological correlations of this process, on the assessment of the risks of complications and/or the stage of complications. It is proposed to consider the possibility of changing the term obesity itself (for example — chronic disease of adipose tissue — adiposity-based chronic disease (ABCD).Thus, today there is a shift from assessing obesity based on BMI (BMI-based approach) to assessing obesity based on the presence or absence of obesity-related diseases or conditions (complication-based approach). A 4-step approach is recommended for assessing all patients:
- screening with BMI adjusted for ethnic differences;
- clinical assessment for obesity-related complications using a checklist;
- assessing the severity of complications using specific criteria and
- selection of preventive measures and/or treatment strategies targeted at specific complications.
The main goal of treatment is proposed to be considered not to reduce the BMI, but to improve the quality of life, prevention and treatment of the consequences of obesity-associated conditions and diseases. Treatment recommendations include lifestyle modification for stage 0 obesity; in the 1st stage of obesity, additional behavioral therapy in combination with or without drug therapy for obesity. A good effect is considered to be a weight loss of 3-10%. Medical therapy for weight management is considered appropriate for BMI over 27 kg/m
2.

2, the expediency of bariatric surgery (various types of operations, including endoscopic ones, to reduce the volume of the stomach) is additionally considered. A good effect at this stage is considered to be a weight loss of more than 10%. At the same time, it is noted that obesity is a complex problem and cannot be effectively managed with simple solutions.
Thus, despite a huge number of studies that have confirmed over several decades the relationship of overBMI and obesity with chronic noncommunicable diseases, the predictive value of BMI has not been definitely established.There are many unresolved problems and controversial issues regarding the assessment and management of various population groups of healthy and sick people against the backdrop of a global trend towards an increase in the number of people with excess BMI. The widely discussed “obesity paradox” led to the emergence of a new paradigm for assessing obesity among US endocrinologists.
The accumulated information deserves attention and discussion by domestic specialists with the creation of interdisciplinary recommendations (endocrinologists, cardiologists, therapists) on the tactics of managing patients and persons with risk factors for chronic diseases.
According to







Add a comment