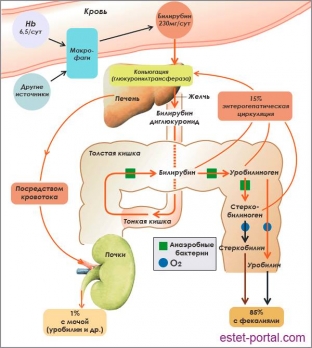
Bile pigments are products of heme breakdown. The primary product of catabolism is gemma-tetrapyrrole. It is converted into bilirubin in the body with the help of enzymes. These substances do not dissolve in water. Together with blood proteins – bilirubin enters the liver with albumin and is conjugated. Conjugation in the liver converts bilirubin to a water-soluble substance, and this happens through a reaction with & nbsp; glucuronic acid. Bilirubin is secreted into bile, which enters the intestines and is thus excreted from the body.
Mechanisms and goals of bilirubin conjugation in the liver
Free bilirubin, which comes from the blood to the liver, binds to glucuronic acid. This process occurs in the smooth endoplasmic reticulum with the participation of a set of enzymes UDP-glucuronyltransferase and UDP-glucuronic acid. In this case, mono- and diglucuronides are synthesized. Bilirubin-glucuronide is direct, conjugated or conjugated bilirubin.
After the formation of conjugated bilirubin, it is released into the bile ducts by an ATP-dependent transporter. When ingested, bacterial β-glucuronidase converts bilirubin to free bilirubin. At the same time, a small amount of direct bilirubin can enter the blood from bile through intercellular spaces. Thus, two forms of bilirubin are simultaneously present in the blood plasma - direct and indirect.
Conversion of bilirubin in the intestine. Types of bilirubin
When it enters the intestine from the bile ducts, conjugated bilirubin is exposed to the intestinal microflora, and direct bilirubin is converted into mesobilirubin and mesobilinogen (urobilinogen). Some of these compounds enter the bloodstream and are transported to the liver. In the liver, mesobilirubin and urobilinogen are oxidized to di- and tripyrolles. In a healthy and normally functioning body, such bilirubin compounds do not enter the urine and blood of a person. They completely remain in the liver cells. The residual part of bilirubin in the large intestine under the influence of microflora is converted into stercobilin, which stains the stool brown. Thus, bilirubin is excreted from the body.
Elevated bilirubin due to impaired conjugation
With a decrease in the activity of bilirubin glucuronyl transferase, the process of bilirubin conjugation in the liver is disrupted and increased bilirubin is observed due to indirect bilirubin. This process is observed in newborns in whom the enzyme does not yet function properly. At the same time, the skin and sclera turn yellow, and the level of bilirubin in the blood is not higher than 150 mg / l. This condition is physiological and passes without a trace in the second week of life. In premature babies, jaundice sometimes drags on for up to 4 weeks. In this case, the level of bilirubin can reach about 200 mg / l. This situation is dangerous because bilirubin encephalopathy may develop.
There is also a disease that prevents glucuronyl transferase from maturing. This is a disease of the thyroid gland – hypothyroidism. Bilirubin in hypothyroidism can reach 350mg/L.
Hereditary disorders of bilirubin conjugation in the liver
There are pathologies and syndromes that are accompanied by defects in the synthesis of glucuronyl transferase and a violation of the process of conjugation of bilirubin in the liver.
- Crigler–Nayar Syndrome, which has two forms. Type 1 - complete absence of glucuronyltransferase, type 2 - partial deficiency of the enzyme. This syndrome is inherited in an autosomal recessive manner. Type 1 can cause an increase in the concentration of bilirubin in the blood up to 340 mg / l. In children of the first year of life, the syndrome can cause kernicterus, which sometimes leads to death. With Crigler-Nayar syndrome, phototherapy is effective, which can reduce the level of bilirubin by up to 50%. But in subsequent periods, the development of nuclear jaundice is possible.
In the second type of syndrome, hyperbilirubinemia is less high. The types of Crigler-Nayar syndrome can be distinguished by the effectiveness of treatment with phenobarbital. In the second type, the level of bilirubin and the part of unconjugated bilirubin decrease, and the content of mono- and diconjugates in bile increases. In the first type, the concentration of bilirubin in the blood serum does not decrease.
- Dubin-Johnson syndrome is a chronic benign jaundice characterized by the presence of dark pigment in the centrilobular region of hepatocytes. Often such a liver is called "chocolate". With the syndrome, defects in the secretion of bile, porphyrins and dark pigment are noted. The development of the syndrome is provoked by a violation of the transport of organic anions into the bile. Dubin-Johnson syndrome is not accompanied by itching of the skin, and the level of bile phosphatase and bile acids remains normal.
- Rotor Syndrome – This is a familial idiopathic disease in which there is an equal increase in direct and indirect bilirubin. Rotor syndrome is very similar to Dubin-Johnson syndrome, however, it does not show dark pigment in hepatocytes. With this pathology, the uptake of unconjugated bilirubin by liver cells is disrupted. The syndrome is manifested by chronic jaundice, icterus of the skin and mucous membranes.
Causes of acquired elevation of bilirubin in the liver
Acquired disorders of glucuronyltransferase activity can be triggered by certain medications and liver pathology. Damage to the liver cells leads to a decrease in excretion function more than the function of bilirubin binding. Therefore, with liver disease, bilirubin is always elevated, mainly due to conjugated bilirubin.
- Hyperbilirubinemia due to excess of direct bilirubin in the blood. Violation of the release of bilirubin into the bile ducts leads to hyperbilirubinemia and hyperbilirubinuria. When bilirubin is detected in the urine, this indicates an increased content of direct bilirubin in the blood. This analysis determines the type of jaundice. After all, jaundice occurs against the background of obstruction of the bile ducts and against the background of hepatocellular diseases.
- Acquired dysfunction of the glucuronyltransferase enzyme occurs while taking medications that affect the structure and function of hepatocytes.
Also, liver diseases, such as cirrhosis and hepatitis, provoke violations of enzyme activity. When liver cells are damaged, ducts appear between the bile ducts, blood and lymphatic vessels, through which bile enters the blood. The hepatocytes swollen due to the pathological process compress the bile ducts and cause obstructive jaundice.







Add a comment