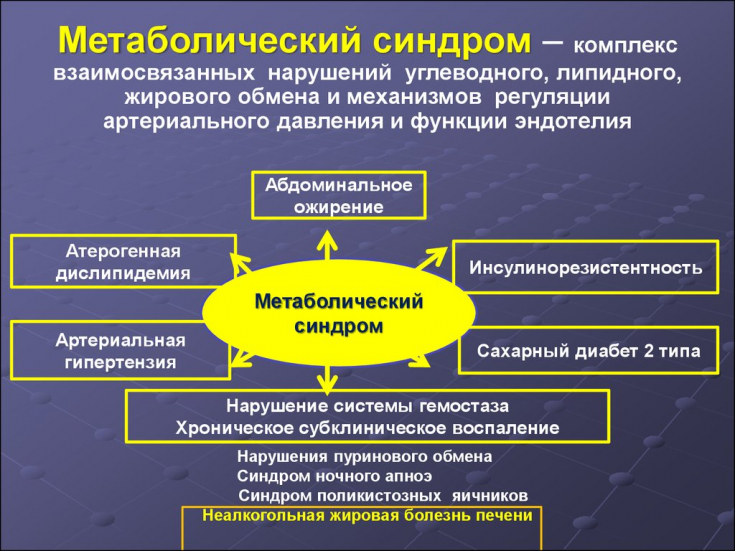
An unusual second name for the metabolic syndrome − "death quartet", due to the fact that the disease has four main manifestations:
- increased blood pressure;
- obesity and overweight;
- increased levels of cholesterol and triglycerides in the blood;
- second degree diabetes mellitus, impaired glucose tolerance and insulin resistance.
Therefore, metabolic syndrome − a problem that is of great interest to both endocrinologists, cardiologists, and therapists, nutritionists and other specialists.
Learn in the article on estet-portal.com about the pathogenesis of metabolic syndrome and the main approaches to therapy for this disease.
- The main components of the metabolic syndrome
- Insulin resistance as a specific disorder of the metabolic syndrome
- Metabolic Syndrome Therapya
The main components of the metabolic syndrome
Metabolic syndrome X, as a separate concept, was introduced into scientific terminology under the name "metabolic tri-syndrome" (trisyndrome metabolique) by JP Camus in 1966
"Abundance Syndrome" − this name was given to this syndrome by H. Mehnert and H. Kuhlmann in 1968
Later, this complex of disorders was given the name "metabolic syndrome".
Follow us on Instagram!
New data obtained during the study of the pathogenesis of the metabolic syndrome made it possible to identify the following components:
- Insulin resistance (decrease in insulin-dependent glucose utilization by tissues).
- Hyperinsulinemia (compensatory mechanism).
- Impaired glucose tolerance, later − violation of carbohydrate metabolism (hyperglycemia on an empty stomach > 5.5 mmol / l).
- Abdominal obesity (BMI > 25 kg/m2 in women and > 27 kg/m2 in men).
- Hypertriglyceridemia (> 2.2 mmol/L).
- Low high-density lipoprotein (HDL) levels (
International guidelines for the treatment of obesity in children
- Hypertension (> 140/90 mmHg).
- Ischemic heart disease (CHD).
- Microalbuminuria.
- Hyperuricemia (> 0.383 mmol/L).
- Decrease in blood fibrinolytic activity.
- Hyperleptinemia and leptin resistance.
Note: blood glucose concentrations are given in capillary whole blood, lipid and uric
is the pathophysiological basis of the metabolic syndrome and subsequent disorders that play a leading role in the pathogenesis of hypertension, coronary heart disease and non-insulin dependent diabetes mellitus (type II).
− primary selective and specific violation of the biological action of insulin, accompanied by a decrease in glucose uptake by tissues (mainly skeletal muscles), and leads to chronic compensatory hyperinsulinemiai.
Risk factors for the development of insulin resistance are: genetic predisposition, obesity, physical inactivity, old age.Therapy of metabolic syndrome
In the treatment of patients with metabolic syndrome, the question of the possibility of influencing
tissue insulin resistance and hyperinsulinemia− general mechanisms that cause this pathology. Theoretically, it is possible that improving tissue insulin sensitivity and reducing chronic hyperinsulinemia, at least in individuals without severe manifestations of arterial hypertension, atherosclerosis, or type 2 diabetes, can break the
"vicious circle"characteristic of them metabolic disorders.
How cortisol levels affect a person's quality of life Insulin resistant persons, regardless of the presence or absence of pronounced clinical manifestations of these diseases, should definitely take preventive or therapeutic measures.
Given the need for
antihypertensive, antianginal and other cardiovascular drugs in insulin resistant patients, preference should be given to those that improve tissue insulin sensitivity and carbohydrate tolerance.
Metformin
:increases the affinity of insulin receptors for insulin;
- increases phosphorylation;
- normalizes the activity of insulin receptor tyrosine kinase;
- enhances postreceptor insulin signal transduction and translocation of glucose transporters;
- increases muscle glycogen synthesis;
- reduces basal hyperinsulinemia;
- normalizes the 1st phase of insulin secretion;
- reduces basal levels of higher fatty acids;
- suppresses hepatic glucose production;
- increases the half-life of insulin;
- suppresses the effects of glucagon in the liver;
- slows down the absorption of glucose and increases its utilization in the intestine.
- (reduces triglyceride levels, inhibits the synthesis of major cholesterol synthesis enzymes, inhibits lipolysis, increases HDL levels);
- normalizes the state of the blood coagulation system (reduces platelet aggregation, the level of thromboxane, beta-thromboglobulin, blood coagulation factor VIII); activates fibrinolysis processes.







Add a comment