Acute Respiratory Infections (ARIs) comprise a large and heterogeneous group of infections, including bacterial, viral, and combinations thereof. In recent years, procalcitonin, a blood marker of bacterial infections, has emerged as a promising tool for coordinating antibiotic therapy.
Several randomized controlled trials have demonstrated the feasibility of using procalcitonin to initiate and stop antibiotics in a variety of ARI patient populations and settings — from primary care facilities to emergency departments, hospital wards and intensive care units. However, the impact of procalcitonin use on clinical outcomes is unclear.
Refer to estet-portal.com for a detailed 2017 update of the Cochrane Review and individual participant meta-analysis to assess the safety of using procalcitonin as a marker of antibiotic efficacy.
Procalcitonin: origin and association with inflammation
Procalcitonin — a polypeptide that is an inactive precursor of calcitonin. Normally, procalcitonin is formed from preprocalcitonin in C-cells of the thyroid gland under the influence of calcium-dependent factors. In healthy individuals, all procalcitonin is converted to calcitonin and practically does not enter the bloodstream.
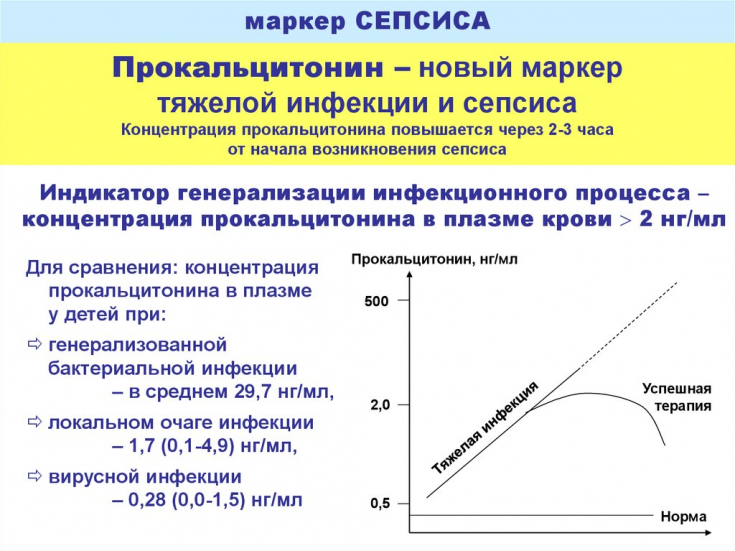
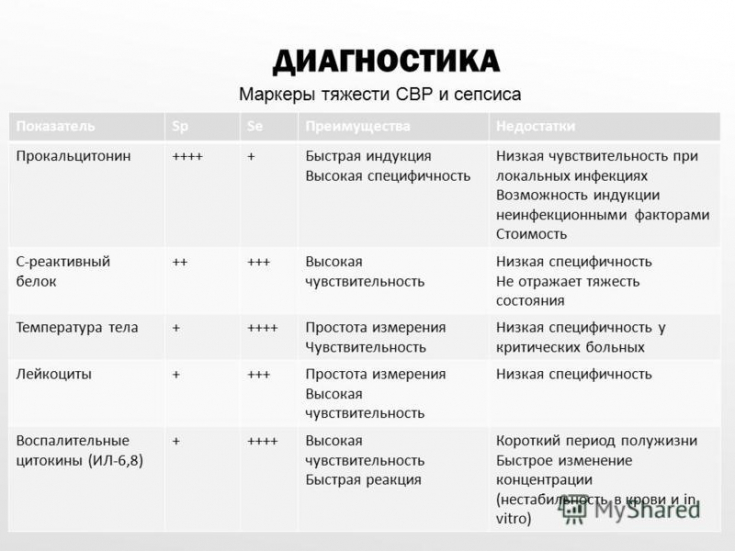
In severe bacterial infections and sepsis, massive endotoxin production, increased levels of the pro-inflammatory cytokines IL-6 and TNF-α; leads to an increase in the synthesis of procalcitonin not only in the thyroid gland, but also extrathyroidally: primarily in leukocytes, monocytes, as well as in neuroendocrine cells of the lungs, intestines and liver.
After 6-12 hours after the generalization of the infectious process, a rapid and sharp increase in procalcitonin occurs.
It must be taken into account that the increase in procalcitonin does not occur with fungal and viral infections, allergic and autoimmune diseases, which allows for differential diagnosis.
Follow us on Instagram
The half-life of procalcitonin is 25-30 hours, which allows it to be used as a marker of the effectiveness of antibiotic therapy (after successful surgical treatment or antibiotic therapy, the level of procalcitonin in the blood quickly decreases by 30-50% per day). On the other hand, with a persistent increase in the level of procalcitonin for more than 4 days, a correction of treatment is needed. If after treatment there is no rapid decrease in the level of procalcitonin, the prognosis of the disease is doubtful.
An increase in the level of procalcitonin above 1.8 ng / ml indicates the development of infectious complications (sensitivity — 80–95%, specificity — 88–93%).
Multicentre Procalcitonin Efficacy Study
Emerging bacterial resistance to antibiotics calls for more stringent measures to reduce the empiric use of antimicrobial agents for uncomplicated, nonbacterial disease and to reduce the duration of antibiotic treatment for clinically resolved bacterial infection.
Today, the problem of competently reducing the empirical use of antimicrobial agents is relevant.
The authors searched the Cochrane Central Register of Controlled Trials (CENTRAL), which contains specialized data from the Cochrane Acute Respiratory Infection Group, MEDLINE and Embase.
32 eligible RCTs with 6708 participants were included. There were 286 deaths in 3336 participants treated with procalcitonin (8.6%) compared to 336 in 3372 control participants (10.0%), indicating a significantly lower mortality associated with the use of procalcitonin in initiation and control of antibiotic therapy (p = 0.037).
Treatment failure was not significantly lower in participants taking procalcitonin (23.0% vs 24.9% in controls, P = 0.068).
Principles for the diagnosis and treatment of mycoplasma respiratory tract infections
Procalcitonin use was associated with a reduction in duration of antibiotic use by 2.4 days (5.7 vs 8.1 days, P < 0.001) and a lower risk of antibiotic-related side effects (16.3% vs 22, 1%, P<0.001).
The length of stay in the hospital and in the intensive care unit were the same in both groups. An analysis of pooled sensitivity data based on all 32 eligible studies showed similar results.
Procalcitonin: a marker of antibiotic efficacy
This updated meta-analysis of data from 12 countries shows that the use of procalcitonin to coordinate the initiation and duration of antibiotic therapy results in a reduced risk of mortality, reduced antibiotic consumption, and reduced risk of antibiotic-related adverse events.
The results were similar across clinical settings and types of ARI, thus supporting the use of procalcitonin in the context of antibiotic management in people with ARI. Future qualitative studies are needed to confirm the results in immunocompromised patients and patients with non-respiratory infections.
Thank you for staying with estet-portal.com. Read other interesting articles in the "Dermatology" section. You may be interested in Abscess and its causes: why asepsis is so important







Add a comment