Traditionally, laser facial skin rejuvenation is associated with resurfacing with CO2 and Er:YAG lasers, in which the rejuvenation effect is due to the destruction of the epidermis and damage to the dermis, leading to the reorganization of its structural components with an intermediate activation of wound healing mechanisms. However, stimulation of collagen and extracellular matrix is possible even with significantly less skin damage, which reduces the risk of complications and reduces the duration of the postoperative period. These studies have led to the widespread adoption of non-ablative skin rejuvenation, also referred to as photorejuvenation.
 Vladimir Alexandrovich Tsepkolenko
Vladimir Alexandrovich Tsepkolenko
MD, Professor, Honored Doctor of Ukraine,
President of the Ukrainian Society of Aesthetic
Medicine, General Director of the Ukrainian
Institute of Plastic Surgery
and aesthetic medicine "Virtus"
Non-ablative photorejuvenation – This is a process in which light energy is used for controlled thermal effects on individual components of the dermis without damaging the epidermis in order to eliminate age-related skin changes (including wrinkles), as well as changes associated with environmental exposure. Rejuvenation occurs as a result of stimulation of the formation of new collagen and the synthesis of the extracellular matrix. In addition, non-ablative rejuvenation should include the elimination of secondary signs of age-related skin changes that are not exclusively structural (superficial dyspigmentation, telangiectasia, hirsutism, rosacea).
Thus, we have characterized two types of non-ablative photorejuvenation: the first involves structural changes in collagen and connective tissue and is aimed at reducing wrinkles, pores, and elastosis; the second is used for vascular, pigmentary and inflammatory phenomena associated with involution-dystrophic changes in the skin.
All sources of energy currently used for photorejuvenation are united by the use of skin chromophores as foci of thermal damage, around which the production of new collagen is stimulated and the subsequent restoration of damaged collagen with stimulation and restoration of fibroblasts. However, other photorejuvenation mechanisms are currently known. Inflammatory cytokines, resulting from cell injury or necrosis, and a hallmark of wound healing, affect the release of extracellular matrix proteins such as type I collagen, fibronectin, and decorin by fibroblasts. At the same time, skin enzymes (MMP matrix metalloproteinase) are produced that destroy part of the resulting collagen and other components of the extracellular matrix, which promotes tissue remodeling (for example, MMP-1 & ndash; collagenase – prevents excessive formation of type I collagen, presumably by increasing the relative proportion of other types of collagen that do not form fibrils and increase skin elasticity).
The most commonly used lasers in photorejuvenation include:
1. Visible emission range:
- Nd:YAG and Nd:YVO4 frequency doubling lasers, KTP (green 532 nm);
- pulsed dye laser (yellow 585-595 nm);
- ruby laser (680 nm).
2. Infrared radiation range:
- diode lasers (800-950, 1450 nm);
- Nd:YAG and Nd:YVO4 lasers (1064 nm);
- Nd:YAG laser (1320 nm);
- Er:glass laser (1540 nm).
The first category includes lasers in the visible range, the radiation of which is mainly absorbed by hemoglobin and melanin. These lasers are mainly used to treat secondary age-related changes (telangiectasia, pigmentation, hirsutism, acne) (Table 4).
Recommendations for the use of non-ablative skin rejuvenation in various age-related changes
| Aging changes | Laser type |
| Telangiectasias | Nd:YAG and Nd:YVO4, KTP, 532 nm |
| Pigmentation | Ruby, 680 nm; alexandrite, 755 nm |
| Shallow wrinkles | Nd:YAG, 1064 nm; diode laser, 810 nm |
| Wrinkles of medium depth | Nd:YAG, 1064, 1320 nm; diode, 1450 nm; Er:glass, 1540 nm |
| Fresh acne breakouts | Alexandrite, 755 nm; diode laser, 810 nm |
Second category – sources of infrared radiation, absorbed equally by hemoglobin, melanin and water (with increasing wavelength, the percentage of absorption by water increases significantly). Infrared waves are used to thermally damage the dermis and trigger the neocollagenesis reaction.
When choosing a specific laser, it is necessary to know what effect its radiation actually has on tissues, and not exaggerated data from manufacturers. Knowing the power of the device, the chromophore that absorbs energy (hemoglobin, melanin, water or all together), as well as the spot diameter and pulse parameters, the doctor can choose the most appropriate laser system for each specific case. For example, it is impossible to carry out photorejuvenation of a pigmented formation with a device with a wavelength of 1450 nm, since in this case the energy is mainly absorbed by water, and not by melanin.
Fractional photothermolysis
Fractional rejuvenation is a new laser treatment method that creates multiple areas of heat damage – microthermal treatment zones (MLZ) (Fig. 2.5-20), surrounded by intact areas of the epidermis and dermis. Intact skin areas allow rapid repair of microscopic damage (Fig. 2.5-21), allowing high-energy treatment with minimal risk of side effects.
After photocoagulation during the day, viable cells move from the periphery of the MLZ, aseptic inflammation develops at the site of the MLZ, during which necrotic fragments of cells and extracellular structures are partially phagocytosed by macrophages migrating to the inflammation zone. 1 hour after the end of irradiation, clearly defined columns of epidermal and dermal damage are determined, and the overlying stratum corneum remains intact. The resulting microscopic epidermal necrotic remnants consist of damaged epidermal and dermal cells, as well as melanin and elastin. These particles are extruded transepidermally between days 3 and 7 after laser treatment. Cellular markers of wound healing and new collagen synthesis were found inside the treated areas:
The proliferative stage of inflammation that has developed at the site of MLZ includes the synthesis of new structural elements of the epidermis and dermis, as well as the reorganization of the surrounding space. The healing process differs from that observed with other methods, since the intact skin zones located between the MLZ contain a large number of viable cells, intraepidermal stem cells and fibroblasts. Thus, the restoration of the skin microstructure in the affected area occurs quickly, with minimal side effects.In clinical terms, fractional resurfacing results in high-quality clinical results, often similar to ablative lasers, without side effects such as permanent hypopigmentation or scarring.
Unlike other non-ablative lasers, non-ablative fractional photothermolysis can be safely used without refrigeration due to microscopic treatment areas, minimizing the risk of extensive heating. However, in practice it is often necessary to resort to cooling means in addition to preliminary local anesthesia due to palpable and sometimes significant pain during processing. The most commonly used devices are forced air cooling.
Fractional ablative photothermolysis
Fractional CO2 and Er:YAG lasers have been developed to achieve clinical results comparable to conventional ablative lasers. These devices provide ablation of the epidermis and thermal damage to the dermis of various depths, which contributes to a more pronounced healing response and concomitant dermal fibrosis. As a result, there is a more significant clinical effect compared to non-ablative technologies, and the healing time and the risk of scarring are significantly less than with conventional ablative lasers.
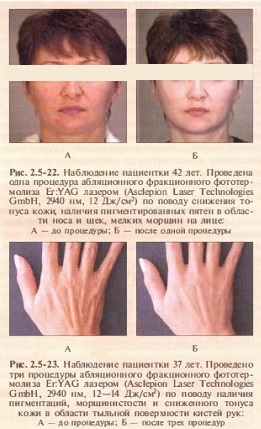
Ablative Fractional Lasers provide clinically visible improvement in facial wrinkles, photodamage, post-acne, and skin elasticity even after a single treatment session. Unlike traditional ablative lasers, it is possible to carry out the treatment only under local anesthesia and without intensive cooling. Fractional ablation does not cause exudation, and it takes 1-2 days to care for an open wound surface. If there is a history of recurrent herpes simplex, antiviral prophylaxis is recommended before the procedure. It is also possible to take prophylactic antibiotics if indicated. Hypopigmentation and permanent scarring are not noted (Fig. 2.5-22, Fig. 2.5-23).
Non-ablative technologies for skin rejuvenation restore the structure of the dermis without significant damage to the epidermis.
Exposure to radiation in the range of 1064-1450 nm
improves the appearance of the skin, its structure and function through the formation of new collagen and the synthesis of the extracellular matrix without damaging the epidermis.Non-ablative fractional photothermolysis
has significant clinical efficacy, can be applied to any area of the body, and treat patients with all skin types according to Fitzpatrick.The most effective and at the same time the safest way to correct age-related changes (both primary and secondary) is method of ablative fractional photothermolysis
, which provides renewal of the skin microstructure and a short rehabilitation period for patients.To be continued.









Add a comment