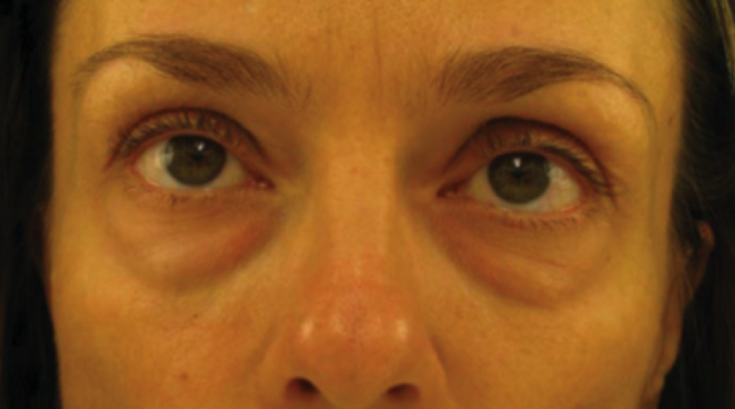
The appearance of the nasolacrimal sulcus is not necessarily due to aging, however, age-related changes in the architecture of the surrounding soft tissues entail an increase in its depth and severity. Dark circles and hollows under the eyes, tired appearance – typical complaints accompanying the appearance of the nasolacrimal groove. Previously, chemical peels and surgical procedures were most often used to correct this cosmetic defect.
They have been replaced by less invasive techniques for volume replenishment with fillers, most often – based on hyaluronic acid. Complications of contouring in the periorbital zone occur more often than in other areas of the face.
Because knowledge of anatomy of soft tissues and blood vessels, which will be discussed in the article estet-portal.com, – basis for safe filling of nasolabial folds.
- Nasal, palpebromalar and midcheek sulci
- What factors influence the formation and severity of the nasolacrimal sulcus
- Anatomy of the nasolacrimal trough: muscles and ligaments
- Anatomy of the nasolacrimal trough: fat compartments
- Anatomy of the nasolacrimal trough: blood vessels
- Anatomy of the nasolacrimal trough: lymphatic vessels
- Recommendations for filling the nasolacrimal sulcus with fillers
Nasal lacrimal, palpebromalar and mid-cheek sulci
Nasolacrimal sulcus – the medial third of the depression that runs from the inner corner of the eye to the midline of the pupil in the infraorbital region. This structure consists of thin and less elastic eyelid skin, as well as denser cheek skin. Along the nasolacrimal sulcus, the fascia attaches to the underlying periosteum.

The palpebromalar groove is located more lateral. In patients with deep nasolacrimal and palpebromalar grooves, an almost continuous depression is formed, which is visualized several millimeters below the edge of the orbit.
The medial buccal sulcus is located below and
pigmentation;
- protrusion of fat pads;
- appearance of wrinkles.
excessive ultraviolet exposure;
- birthmarks;
- melanoma;
- dermal melanocytosis;
- diseases (systemic and skin);
- sleep disorders;
- Nutritional deficiency.
- Dispigmentation does not affect the actual depth of the nasolacrimal trough, but increases it visually.
In case of hyperpigmentation in the infraorbital region, in addition to filling the nasolacrimal trough with fillers, additional correction methods may be required.
The formation of the nasolacrimal sulcus is often associated with protrusion of orbital fat in the lower eyelid area. At the same time, fatty hernias of the lower eyelid present a separate problem.Orbital fat prolapse
can be identified by the characteristic shape of the orbital fat compartments, which often show through the skin, the central fat compartment shaped like a cigar. Follow us on
Instagram! In patients with severe fat pad prolapse, monotherapy with dermal fillers may be contraindicated. Lower blepharoplasty may be an alternative in such cases.
Appearance of
wrinkles on the skin of the lower eyelidcan also increase the severity of the nasolacrimal sulcus. Characteristic features of this zone:
minimum amount of subcutaneous fat;- thinned skin;
- Dynamism due to the activity of the orbicular muscle of the eye.
Loss of volume in the central third of the face
also increases the severity of the nasolacrimal sulcus due to:
loss of anterior projection of the maxilla;- omissions and atrophy of malar
fat packs. - Anatomy of the nasolacrimal trough: muscles and ligaments In the subcutaneous plane, the nasolacrimal and palpebromalar sulci do not separate. The anatomical nasolacrimal groove is located on the orbital ridge, in its most medial part, and the depression runs along the fibers of the circular muscle of the eye. In this position, the muscle is directly connected to the lower part of the eye roller. Subcutaneous tissue is poorly expressed between the skin and muscle in this zone.
Infraorbital furrows and cavities: Filler correction technique The origin of the levator lip is located in the medial part of the ophthalmic ridge, directly below the insertion of the orbital part of the orbicularis oculi muscle. The space between these two muscles is located below and medial to the sulcus.
Laterally, in the central part, the sulcus runs at the maximum distance from the orbital ridge. The orbicular muscle of the eye is attached to the bone by retaining ligaments at the junction of the eyelid and cheek. The ligament holding the orbicular muscle of the eye attaches to the zygomatic bone caudally to the marginal artery at the orbital ridge. The fibers of the ligament also pass superficially, separating the preseptal and orbital parts of the orbicularis oculi muscle. The length of the fibers of the retaining ligaments maximizes in the center, at the arcuate expansion of the orbital septum, and is minimized, merging with the lateral orbital thickening in the region of the outer corner of the eye. Retaining ligaments form a v-shaped deformity that corresponds to the connection of the eyelid and cheek zones.

Soft tissue atrophy and weakening of the orbital ligament leads to protrusion of orbital fat through the secular part of the circular
The orbital fat provides the gliding plane of the eyelid and eyeball. There are two fat pads in the upper eyelid:
nasal;
central (preaponeurotic).
- There are three of them in the lower eyelid:
central;
lateral.- Read also: Lacrimal trough filling: a case report
The nasal and central compartments are separated by the inferior oblique muscle of the eye, which elevates the eye and rotates it outward. Orbital fat pads are held in place by the orbital septum, which weakens with age. As a result, hernias of infraorbital fat pads can form. The infraorbital fat is located deep under the orbicular muscle of the eye in the region of the zygomatic eminence. The gradual descent of this fat pack under the influence of gravity plays an important role in the downward displacement of the soft tissues of the middle third of the face and periorbital zone. Anatomy of the nasolacrimal trough: blood vessels
Ocular artery (HA) – the main vessel that provides blood supply to the orbit. This is the first branch of the internal carotid artery, which originates after exiting the cavernous sinus and enters the orbit through the optic canal. However, cases are known when the ophthalmic artery emerges from the middle meningeal branch of the external carotid artery and enters the orbit through the superior orbital fissure.
The vasculature of the periorbital zone is characterized by a high degree of individual variability.
GA branches can be divided into two groups:
Orbital:
tearful;
- supraorbital;
- posterior ethmoid;
- internal artery of the eyelids;
- frontal (terminal branch);
- nasal (terminal branch).
- Ocular:
- short lash;
- central retinal artery;
- muscular.
- Only a small proportion of the orbital blood supply comes from the carotid artery (through its infraorbial branches) and the ophthalmic branch of the middle meningeal artery.
- Occlusion of the long and short anterior and posterior ciliary arteries can lead to symptoms of anterior ischemic optic neuropathy, including vision loss
.
The orbit is surrounded by an extensive network of vascular anastomoses. The literature describes in detail the anastomoses between the branches of the internal carotid artery, as well as the temporal arteries and arteries of the orbit. Occlusion of any of these may result in loss of vision. Anatomy of the nasolacrimal trough: lymphatic vessels
The lymphatic vessels of the periorbital zone are classified into pretarsal and posttarsal. Lymphatic vessels of the periocular zone are divided into pre- and posttarsal. The outflow of lymph from the pretarsal part of the circular muscle of the eye and the skin of the eyelids is carried out through the pretarsal lymphatic vessels, and from the conjunctiva, lacrimal glands and tarsal plates – along the deep plexus of posttarsal vessels.
Lymph outflow from palpebral lymphatic vessels is carried out by:
laterally (into the deep and superficial parotid nodes) – from the lacrimal glands of the conjunctiva, the lateral parts of the eyelids;
medially (to the submandibular lymph nodes) – from the medial parts of the eyelids and lacrimal sacs.
- Recommendations for filling the nasolacrimal trough with fillers
- To fill the nasolacrimal trough, fillers with low viscosity and elasticity – they are soft and evenly integrated into the tissues.
Highly cross-linked HA fillers are not used to correct the nasolacrimal trough, as they are more likely to cause swelling, impairing lymph flow.
Read also:
Filling the nasolacrimal trough with hyaluronic acid through one point
When working with the nasolacrimal sulcus, the hydrophilicity of hyaluronic acid fillers should be taken into account. No need to strive to get the perfect result during the – it will build up over several weeks as the gel attracts water. To avoid overcorrection, it is necessary to undercorrect the nasolacrimal trough during the procedure. It is also worth remembering that small-caliber cannulas, like needles, carry a high risk of vascular damage.
To prevent the occurrence of the Tyndall effect and avoid the appearance of irregularities, it is important to inject the filler with a needle at the level of the periosteum with a needle and cannula – in the plane of the infraorbital fat.
Adapted from Aesthetics.
More interesting videos on our
YouTube
-channel!







Add a comment