Psoriasis – a prime example of collaboration between clinicians and scientists in an attempt to find safe and effective treatments for genetic disorders of the skin, joints and immune system. In some cases, incidental clinical observations led to laboratory work that explained the pathogenesis of this disorder; in other cases the therapy was based on successful experiments in the laboratory.
The result has been a dramatic improvement in our understanding of the pathogenesis of this disorder and our ability to treat patients suffering from psoriasis. In the article estet-portal.com you can get acquainted with the stages of revealing the secret of pathogenesis of psoriasis.
The first cause of psoriasis – abnormal proliferation of keratinocytes
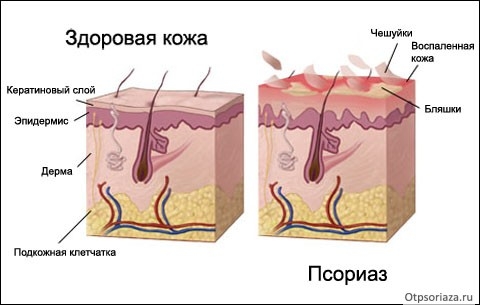
At first, psoriasis was thought to be a major disorder of the keratinocyte. In 1968, Weinstein, van Scott and Frost demonstrated the abnormal proliferation of keratinocytes in psoriasis. Desquamation of psoriatic epidermis has been shown to be markedly faster than normal epidermis.
Simultaneously, van Scott, Auerbach and Weinstein showed that methotrexate is effective in psoriasis, presumably by inhibiting rapidly dividing epidermal cells.
In 1977, Parrish, Fitzpatrick and colleagues introduced a combination of psoralen and ultraviolet light therapy (ultraviolet A – UVA) (photochemotherapy – PUVA). In 1979, it was suggested that PUVA cross-links DNA strands, and again the main effect is to inhibit keratinocyte proliferation.
Only years later did we evaluate the effects of methotrexate and PUVA on the immune system.
Watch the most interesting videos on our channel in Youtube
The second cause of psoriasis – proliferation of keratinocytes and activation of T-lymphocytes
The involvement of the immune system in the pathogenesis of psoriasis was first appreciated in 1988 from the incidental observation that transplant patients who had psoriasis and were treated with cyclosporine experienced regression of skin disease. Griffiths and Voorhees were among the first (1990 and 1989, respectively) to note that the beneficial effect of cyclosporine on psoriasis was due to the drug's effect on T-lymphocytes.
Cyclosporin reduces the number of immune cells, including T-lymphocytes, monocytes, macrophages and antigen-presenting cells.
In 1990, working with an illustrious group of scientists, Gottlieb and Nikoloff and Griffiths demonstrated the many changes in the immune system from cyclosporine therapy and suggested that when T cells are activated, affected T cells release lymphokines that promote keratinocyte proliferation.
The third cause of psoriasis – activation of T-lymphocytes
The role of lymphocytes was convincingly demonstrated when, in 1995, a group led by James Krueger successfully treated psoriasis using a lymphocyte-selective fusion protein composed of interleukin-2 and fragments of diphtheria toxin.
The latter compound selectively blocks activated lymphocytes, but does not affect keratinocytes.
Eight out of 10 patients treated with two doses of this fusion protein had moderate to significant improvement, confirming the role of lymphocytes.
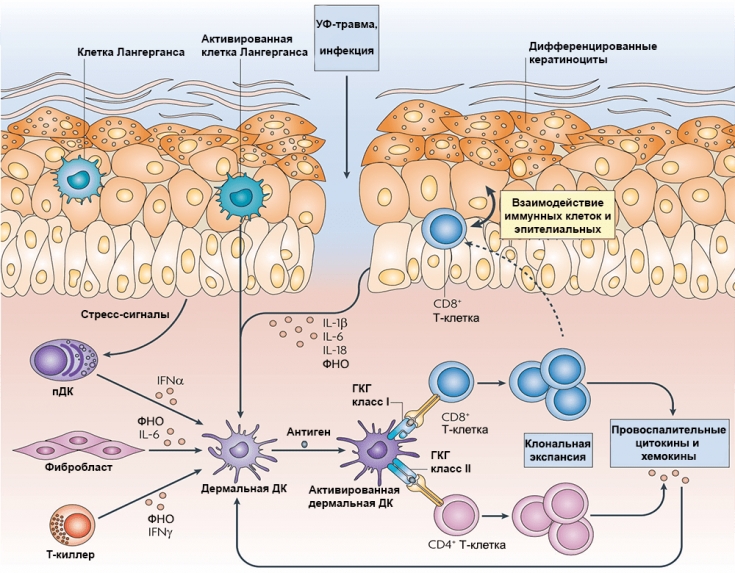
T cell activation has been known to require not only antigen presentation to T cells, but costimulation with a range of possible signals.
CTLA-4 immunoglobulin, now known as Abatacept, is a fusion protein consisting of the Fc portion of human IgG1 fused to the extracellular domain of CTLA-4 (cytotoxic T-lymphocyte-associated antigen-4). By binding to B7 molecules of antigen-presenting cells, Abatacept prevents the co-stimulatory signal, thereby blocking the activation of T-cells and leading to an improvement in the condition of patients with psoriasis.
Abatacept approved for rheumatoid arthritis, still under consideration for psoriasis and psoriatic arthritis.
Follow us on Telegram
The fourth cause of psoriasis – production of pro-inflammatory cytokines
The role of the Th1 cytokine, IFN-γ, was recognized in 2001. Lymphocyte and T cell activation was thought to play an important role in this cytokine network.
Following clinical observations in 2005, it was proven that TNF-α antagonists; lead to a decrease in IL-1 and IL-8 with a subsequent decrease in the expression of inflammatory genes, including IFN-γ, Stat-1 and granzyme B. The α1β2 integrin antagonist efalizumab also interfered with T-cell function in inflamed skin.

Nestlé and Konrad pointed out back in 2004 that p40 plays an important role in psoriasis. This led to the development of two p40-targeting antibodies ustekinumab and briakinumab. Both biologics that target the p40 components of IL-12 and IL-23 were significantly effective, but due to the small increase in myocardial infarctions, briakinumab was not approved in the main studies.
In 2009, we learned that IL-23 activates Th-17 cells to make more IL-17. At least three antibodies that target IL-17 or its receptor have been clinically studied. The first of these, the recently approved Seukinumab, targets IL-17A and proved extremely effective in the treatment of psoriasis in 2014. Ixekizumab – another antibody to IL-17A, is equally effective as brodalumab, an antibody to the IL-17 receptor.
Prospects for further research
Over the past five decades, advances in our understanding and treatment of psoriasis have been driven by close collaboration between scientists and clinicians, making psoriasis a disease model where key scientists and laboratory clinicians benefit from interacting with each other. Advances in the lab have translated into new treatments that are more targeted, profoundly effective, and safer than older treatments. The next frontier in psoriasis is likely to involve pharmacogenomics or, in the distant future, even gene therapy.
In 2001, 2007 and 2010, work was done to identify genes associated with psoriasis.
Thank you for staying with estet-portal.com. Read other interesting articles in the "Experts" section. You may be interested in Psoriasis treatment: experience with vitamin D
Adapted from Journal of Investigative Dermatology







Add a comment