Among all environmental factors, solar ultraviolet radiation (UVR) is the most significant factor for premature skin aging. Other factors include exposure to 760-1440 nm infrared radiation (IRR) from natural and artificial sources, tobacco smoke, and exposure to particulate air pollution.
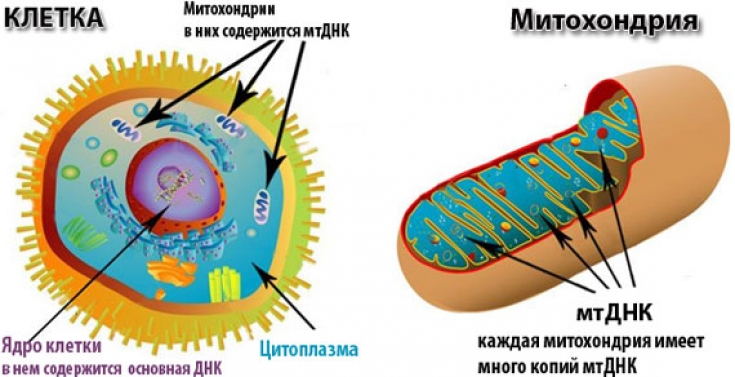
In the case of infrared radiation, oxidative stress is generated inside the mitochondria, which initiates a retrograde signaling reaction that is directed from the mitochondria to the cell nucleus.
In other words, all of these environmental factors cause clinical, histological and even molecular damage in the skin, and are susceptible to prevention strategies.
In this estet-portal.com article, we will focus on the most popular pathogenic concepts of UV-induced skin aging.
Mitochondrial DNA mutations in photoaging
As a result of oxidative phosphorylation (electron transport chain) in mitochondria, energy is synthesized, a by-product of this process are reactive oxygen species. In the immediate vicinity of this site is the mitochondrial own genomic material, mitochondrial (mt) DNA. Despite the repair mechanisms associated with oxidative damage, the mutation rate of mtDNA is about 50 times higher than that of nuclear DNA.
Intra-individual comparative studies have shown that the total deletion, mtDNA deletion, increases 10-fold in UV-exposed skin.
The number of total deletions does not correlate with chronological aging, so mtDNA mutations only reflect the detrimental effects of UV exposure.
Follow us on Facebook
The role of matrix metalloproteinases and collagen synthesis in the process of photoaging
UVR leads to increased and accelerated degradation and a decrease in the synthesis of collagen fibers. There is an induction of matrix zinc-dependent endopeptidases (MMPs). Each MMP degrades different dermal matrix proteins, for example, MMP-l degrades collagen I, II, and III, while MMP-9, also called gelatinase, degrades collagen type IV, V, and gelatin.
Under physiological conditions, MMPs are part of a coordinate network and are finely regulated by tissue-specific MMP inhibitors (TIMPs). Interruption between MMP activation and suppression of activity by TIMP activation can lead to excessive proteolysis.
UV radiation has been shown to induce MMPs without affecting TIMP expression or activity.
• Long-wave UV (320-400 nm) acts through the formation of reactive oxygen species that trigger lipid peroxidation (LPO), transcription factors and DNA-proton transitions.
• Short-wave UV (290-320 nm) induces arylohydrocarbon receptor transcription factors AP-l and NFkB, which are stimulating factors of MMP genes, the latter leads to the degradation of matrix proteins in human skin.
The action of UV extends mainly to the epidermis, where DNA is damaged in keratinocytes and melanocytes, proteolytic enzymes are synthesized, which then affect the dermis in the second stage.
Topical skin pre-treatment with trans-retinoic acid prior to UV exposure prevents AP-I activation.
UV-induced modulation of vascularization
Under the influence of UV radiation, the venous wall thickens, while perivascular cells become thinner in the severely damaged membrane of the vessel wall, local dilatations appear, corresponding to clinical telangiectasias. In all cases, there is a sharp change in the horizontal pattern of vascularization with dilated and distorted vessels.
Acute and chronic UV exposure significantly increases skin vascularity.
The formation of blood vessels from pre-existing vessels is controlled by fibroblast growth factor, interleukin-S, tumor growth factor beta, platelet-derived growth factor and vascular endothelial growth factor (VEGF).
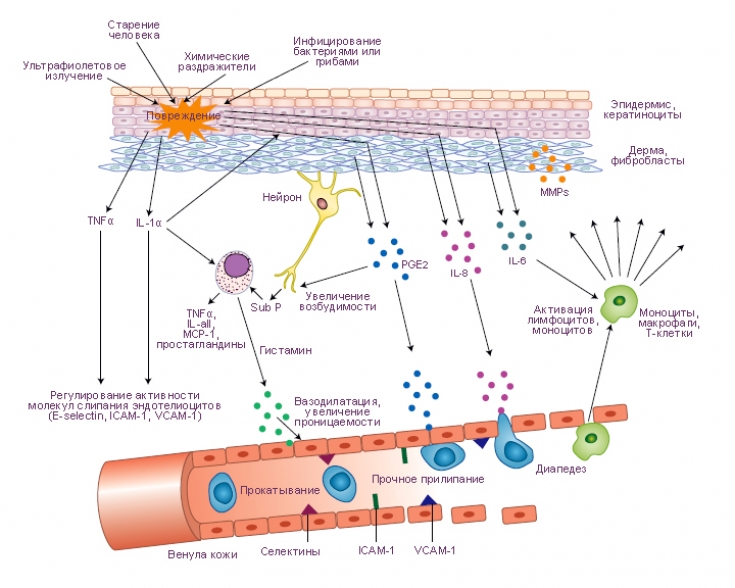
Photoaging as a chronic inflammatory process
Skin that has been exposed to UVR is characterized by an increase in the number of dermal fibroblasts, mast cells, histiocytes, and mononuclear cells. The presence of such a dermal infiltrate indicates chronic inflammation. The terms heliodermatitis and dermatoheliosis have been coined to describe this situation. More recent studies have shown that there is an increased number of CD4+ T cells in the dermis and a decrease in the number of epidermal Langerhans cells.
Sunburned skin: what do we know about actinic dermatitis
Photoaging due to oxidative damage
The aging process is accompanied by increased oxidative damage. Prolein carbonyls can be formed either by oxidative cleavage of proteins or by direct oxidation of lysine, arginine, proline, and threonine residues. In the cell, the proteasome is responsible for the degradation of oxidized proteins. During aging, this function of the proteasome decreases and oxidized proteins accumulate.
In addition, a modified protein aggregate – lipofuscin. This aggregate accumulates inside cells and is able to inhibit the proteasome.
Thus, mitochondrial DNA mutagenesis, telomere shortening, neovascularization, protein oxidation, suppression of collagen synthesis, and increased expression of matrix metalloproteinases are associated with UV-induced premature skin aging.
Thank you for staying with estet-portal.com. Read other interesting articles in the "Cosmetology" section. You might be interested in Effective sun protection: which products to choose







Add a comment