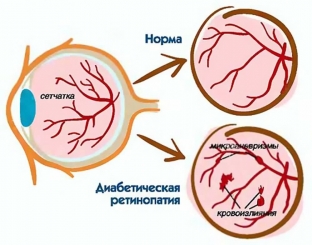
The leading cause of blindness in many countries is diabetic retinopathy. A child with congenital diabetes loses sight at an average of 15 years of age. In the microvascular system of the kidneys and eyes, the same process is reflected in diabetic angiopathy. In connection with the use of insulin for the treatment of diabetes, the prognosis in the treatment of retinopathy has become more favorable. Pathological changes in the fundus of the eye in diabetes mellitus are so pronounced and specific that often the diagnosis of diabetes mellitus is made at an appointment with an ophthalmologist. What fundus changes are indicative of diabetic retinopathy?
What happens in the blood vessels in diabetes mellitus? Pathogenesis of diabetic retinopathy
For successful treatment and prevention of diabetic retinopathy, it is important to know the pathogenetic moments of the formation of retinopathy in diabetes mellitus. The enzyme aldose reductase, together with an increased concentration of glucose in cells, promotes metabolism through the polyol pathway, which provides for the accumulation of sorbitol and fructose. It is these substances that play a decisive role in the death of capillary pericytes and vascular endothelium, after which atony and microaneurysms develop.
Thus, the functioning of many endothelial cells is disrupted along with proliferative processes in other cells. Basement membranes thicken, fibrin is deposited in the walls, increased platelet aggregation contributes to the formation of microthrombi. This is how areas of capillaries are formed that are devoid of perfusion. Against this background, tissue hypoxia develops, which is a source of growth of endothelium, astrocytes and neuroglia.
The above phenomena are the cause of neuroproliferative processes and neovascularization in diabetes mellitus, they occur in absolutely all tissues, including the eye. But it is in the fundus that the earliest signs of diabetic retinopathy are found.
How can early signs of diabetic retinopathy be detected?
An effective way to detect diabetic retinopathy in the early stages is fluorescein angiography of the fundus vessels (FA), which reveals areas of non-perfused capillaries in the subclinical stages of diabetes. This method makes it possible to detect diabetic retinopathy 5-7 years after the onset of the disease in a fifth of patients, after 10 years it is possible to detect changes in the fundus vessels in half of the patients. Retinal changes in diabetes mellitus are very polymorphic.
Pathological changes in the retina in diabetic retinopathy:
- lesion of the choroid and capillaries of the venous system;
- Iris lesion;
- microaneurysm formation;
- increased platelet microaggregation;
- obliteration of vessels, which leads to disruption of tissue respiration;
- retinal vascular thrombosis;
- neovascularization;
- appearance of hemorrhage and foci of retinal opacities;
- appearance of neoplasms of the connective tissue.
What are the early signs of diabetic retinopathy?
Diabetic retinopathy can be identified by a few early signs when examining the fundus. These are waxy exudates, microaneurysms and punctate hemorrhages. Later, preretinal vitreal hemorrhages are visualized, sometimes retinal vein thrombosis can be seen. The presence of proliferative processes with the appearance of new vessels, multiple hemorrhages, retinal fibrosis and proliferation of connective tissue indicates the terminal stage of diabetic retinopathy.
Today, when prescribing treatment for patients with diabetes mellitus, endocrinologists are guided by the degree of damage to the retinal vessels. The effectiveness of the therapy is also evaluated based on the clinical picture of the fundus. Therefore, early detection of diabetic retinopathy is very important for the prognosis of the development of the disease.







Add a comment