The number of women of reproductive and premenopausal age who have had their ovaries removed for one reason or another is steadily increasing. The reason for this is both an increase in the number of inflammatory-destructive and tumor diseases of the uterine appendages, and an increase in the quality of their diagnosis. Surgical treatment is one of the main methods not only in these patients, but also in women with benign tumors of the ovaries and uterus, which is due to oncological alertness, especially in women after 45 years.
But this operation steadily has negative consequences, including on the skin. Read more about dermatological pathology in postovariectomy syndrome at estet-portal.com
- dermatological pathology as a manifestation of postovariectomy syndrome
- dermatological pathology in estrogen deficiency
- replacement therapy as a prevention of the development of dermatological pathology
Dermatological pathology as a manifestation of postovariectomy syndrome
Pathological symptoms after ovarian removal, grouped under the name of postovariectomy syndrome (POES), occur, according to various authors, in 50-80% of women. The duration and severity of symptoms of POES depends on the age of the woman and the initial hormonal status.
Follow us on Instagram!
Since its manifestations are due to estrogen deficiency and the corresponding hyperproduction of gonadotropic hormones (and not only gonadotropic, but also thyrotropic and adrenocorticotropic hormones), a number of researchers believe that POES occurs later in young women, linking this with increased activity hypothalamic structures with age. On the other hand, estrogen deficiency is the leading factor in the pathogenesis of POES, more pronounced in women of reproductive age, with an initially high level of ; therefore, in this category of patients, a severe pathology should be expected.
Read also: Cosmetologist checklist: the most effective cryotherapy techniques
Depending on the time of occurrence, early, medium-term and late symptoms of POES are distinguished:
- early include - menopausal syndrome and myocardial dystrophy,
- to medium-term - dermatological and urogenital symptoms;
- to late - osteoporosis, coronary heart disease and Alzheimer's disease.
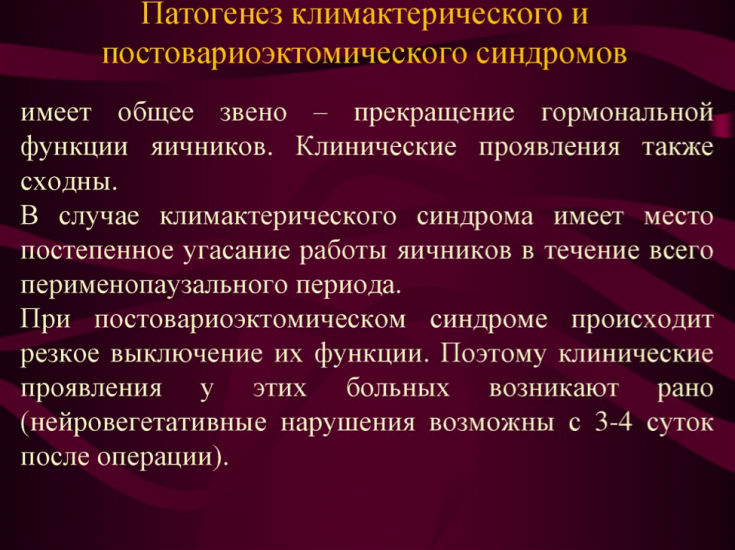
In general, the symptoms and manifestations of POES are similar to natural menopause. However, if menopause is a physiological period of a woman's life, during which, against the background of age-related changes in the body, involutive changes in the reproductive system develop, then surgical removal of the ovaries abruptly terminates the function of the ovaries, and the changes that occur due to the actual hormonal changes. Changes in organs and tissues in POES due to the significant role played by sex hormones in a woman's body.
Dermatological pathology with estrogen deficiency
It has long been believed that the main target organs for sex hormones are the uterus and mammary glands (the so-called reproductive targets).

Today, two large groups of target organs are distinguished - reproductive and non-reproductive, and the second includes:
- cardiovascular and musculoskeletal systems;
- skin and hair;
- urethra and bladder;
- brain;
- large intestine;
- liver.
According to modern data, almost all organs and systems of a woman's body are under the control of sex hormones. This is what determines the diversity and versatility of the clinical symptoms of hormone deficiency conditions associated with both age-related changes and iatrogenic.
Follow us for updates on Facebook!
When studying the effect of estrogens on skin aging processes, B. de Lignieres found that their deficiency reduces the mitotic activity of the cells of the basal layer of the epidermis, reduces the synthesis of collagen and elastin, which causes a decrease in skin elasticity.
Consequently, a decrease in estrogen levels significantly affects the condition of the skin: it becomes thinner, drier, more sensitive, loses elasticity and firmness; wrinkles appear faster.
After an ovariectomy, a decrease in the level of female sex hormones - estrogen and progesterone - can contribute to the development of a relative predominance of male sex hormones in about a quarter of women, which also has an adverse effect on the skin.
Read also: Vascular anatomy of the lips for a beautician
This is one of the pathogenetic links in the appearance of acne vulgaris and seborrhea in women with hyperandrogenism syndrome after postovariectomy.
Replacement therapy as a prevention of the development of dermatological pathology
Thus, in some women, the development of relative hyperandrogenism after postovariectomy may be accompanied by the following dermatological pathology: acne, seborrhea, androgenetic alopecia, hypertrichosis and hirsutism.
Read also: Skin blood supply: what is important for a cosmetologist to consider
A study was conducted in which women receiving hormone replacement therapy had significantly higher collagen content in the skin than a group of patients without therapy.
PG Sator et al studied the effects of estrogen replacement therapy on various skin parameters: surface lipid levels, hydration, elasticity, and skin thickness. As a result of the study, an increase in skin hydration, its elasticity, thickness was found, which was simultaneously accompanied by a clinical improvement in the condition of the skin.
The results of a significant number of studies have convincingly proven that estrogen increases the content of glycosaminoglycans and hyaluronic acid - components of the skin that play an important role in maintaining its turgor. Thus, the hydration of the connective tissue structures of the dermis increases, the skin becomes smoother, as its ability to retain moisture increases.
More useful information on our YouTube-channel:







Add a comment