Herpes zoster – an infectious disease caused by the reactivation of Varicella zoster virus (VZV) after a previous episode of chickenpox. Among patients under the age of 20, the prevalence of the disease is from 0.4 to 1.6 cases per thousand of the population.
In older age groups, the disease is much more common: approximately 4.5-11 cases per thousand population. Accompanied by severe pain and itching, herpes zoster can significantly reduce the quality of life of patients, and sometimes even pose a deadly threat.
Dermatologists, infectious disease specialists, general practitioners, as well as all those who are interested in the latest clinical guidelines for the treatment of diseases of herpes etiology. For more information about the pathogenesis of Herpes zoster development, the clinical picture of the disease, as well as modern approaches to treatment, read on estet-portal.com in this article.
Herpes zoster: key pathogenetic mechanisms of infection development
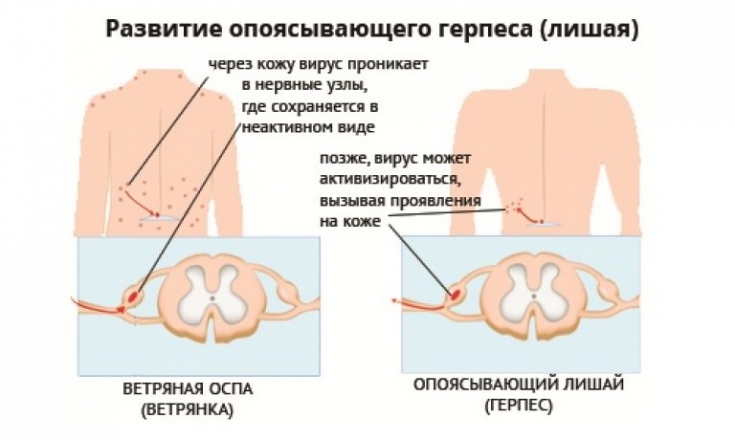
It is common knowledge that primary VZV infection develops as chicken pox. After the disappearance of the clinical manifestations of the disease, the virus persists latently in the human body in the intervertebral ganglia and dorsal roots of the spinal cord.
What is the difference between the rash in different childhood infectious diseases Shingles develops as a result of the reactivation of a latent virus against the background of a decrease in the body's immunological resistance. The latter can be triggered by taking cytotoxic drugs, glucocorticoids, HIV infection, radiation therapy, as well as regular emotional overstrain and poor living conditions of the patient.
Key symptoms of herpes zoster: neuralgia, itching and rashes
The main clinical symptoms of herpes zoster are characteristic rashes, severe neuralgia, itching, as well as weakness and headache. Along the nerves (most often intercostal), pink spots 3-5 cm in size appear, which turn into papules, vesicles and then dry up.
Regional lymph nodes increase in size and become painful. Quite often, the skin of the head and face is affected, especially along the branches of the trigeminal nerve.
Follow us onTelegram Patients with immunosuppression (against the background of taking cytotoxic drugs, glucocorticoids, HIV infection) may develop a gangrenous form of the disease with deep skin lesions and subsequent scarring. Herpes zoster may be accompanied by a lesion of the Gasser node.
In some cases, rashes can be localized along the branches of the trigeminal nerve, as well as on the mucous membranes of the nose, the skin of the face, and even in front of the patient's eyes.
When the eyes are affected, herpes zoster can be complicated by the development of ulcerative keratitis, iridocyclitis, retinal detachment and glaucoma.
In patients with immunodeficiency conditions, as well as those over 60 years of age, it is mandatory to prescribe etiotropic antiviral therapy. In other cases, the question of the appropriateness of its implementation should be decided individually.
Treatment of shingles should be started as soon as possible after the onset of the disease: optimally within the first 72 hours.
In the treatment of herpes zoster, the following etiotropic drugs are used: acyclovir, valaciclovir, foscarnet, famciclovir.
The role of the herpes simplex virus in the occurrence of dermatological diseases The timely administration of etiotropic drugs contributes to the rapid and effective relief of pain in herpes zoster, the elimination of rashes, and prevents the development of postherpetic neuralgia.

In case of herpes zoster, the appointment of etiotropic therapy is mandatory. There are such schemes for the treatment of Herpes zoster:
1. Aciclovir 800 mg 5 po or 10 mg/kg every 8 hours for 7-14 days;
2. Valacyclovir 1 g 3p/d orally for 7-14 days;
If the infection is resistant to acyclovir, one of the following regimens should be used:1. Foscarnet 60 mg/kg IV every 8 hours for 7-14 days, or until the clinical manifestations of the infection disappear;
2. Famciclovir 500 mg twice a day for 7-14 days.The doctor should take into account the possible side effects of some etiotropic antiviral drugs.
To eliminate the pain syndrome in Herpes zoster, it is advisable to use anticonvulsants and analgesics (non-steroidal anti-inflammatory or narcotic analgesics), lidocaine blockades.
The drug of choice is carbamazepine at a dose of 100-300 mg 3 times a day. The drug must be taken until the pain disappears with herpes zoster.
Thank you for staying with estet-portal.com. Read other interesting articles in the "Dermatology" section. You may also be interested in Debilitating itching: modern approaches to the diagnosis and treatment of scabies.









Add a comment