Symptoms of keratoconus appear due to the development of astigmatism and myopia. These processes are accompanied by a progressive decrease in vision and monocular diplopia. As a rule, changes appear first in one eye, and then in the other. Such patients often turn to the doctor for the next selection of glasses. At the same time, wearing glasses does not improve the situation in any way, since visual impairment occurs constantly and progressively. The use of soft contact lenses becomes impossible after some time, since they do not adhere to the cornea. What is the recommended treatment for keratoconus?
Vision in keratoconus. Diagnosis before treatment of keratoconus
A patient with keratoconus sees multi-contour images of objects, there are halos over light sources, letters are distorted when reading. Sometimes there is increased photosensitivity and eye irritation. At the beginning of the disease, twilight vision may be reduced, then vision in illuminated rooms worsens. The patient complains of a constant burning sensation in the eyes, itching and increased fatigue. In advanced stages, if keratoconus is not treated, the corneal deformity is very noticeable.
Progression of keratoconus can last up to 15 years. In half of the patients, the process stops and goes into a stage of long-term remission, despite the lack of treatment for keratoconus. In rare cases, there is a complication – acute keratoconus develops, which is accompanied by a sudden rupture of the descement membrane. In this case, aqueous humor enters the corneal layers. Acute keratoconus is manifested by corneal edema and the presence of pain. The process ends with the formation of scars on the cornea. At the same time, the deformation of the corneal surface may decrease, which improves vision somewhat.
The diagnostic process before treating keratoconus consists of the following tests:
- The examination of the patient begins with a visual acuity test.
- When fitting glasses, an asymmetrically sharp increase in refraction and the need to switch to cylindrical lenses are revealed.
- Skiascopy reveals «valve» shadows due to irregular astigmatism.
- Refractometry detects irregular astigmatism and myopia.
- Diaphonoscopy allows you to determine keratoconus in the form of a wedge-shaped shadow on the iris.
- Signs of conical deformity are determined by ophthalmometry.
- Ophthalmoscopy is performed when the media of the eye are transparent.
Methods of treatment of keratoconus. New method to correct corneal deformity
Based on course and progression, treatment of keratoconus can be non-surgical or surgical. Non-surgical (conservative) treatment consists of vision correction using semi-rigid lenses. These lenses are hard in the center and soft on the periphery. In the initial stages and a stable course, spectacle correction of vision can bring an effect. It is advisable to prescribe courses of tissue therapy, courses of vitamin therapy, antioxidants and immunomodulators, eye drops, parabulbar and subconjunctival ATP injections, and physiotherapy.
A new treatment for keratoconus that has proven itself is called corneal cross-linking. Its essence lies in the removal of the surface layer of the corneal epithelium, after which a solution of riboflavin is instilled, and then irradiated with UV rays. This method of treatment makes it possible to make the cornea resistant to deformation, strengthens it, makes it possible to stop the development of the disease or achieve regression.
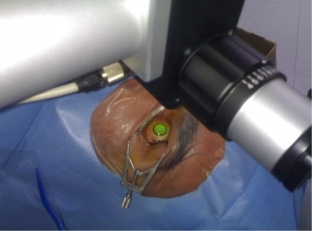
In the surgical treatment of keratoconus, the implantation of corneal rings is used. Classical operations are layered or penetrating keratoplasty, in which the cornea is completely removed and a donor one is implanted.







Add a comment