The lacrimal glands produce a secretion that bathes the eyeball, after which it flows to the inner corner of the eye. It is there that the lacrimal openings leading to the lacrimal canaliculi are located. The tear through them first enters the lacrimal sac, and then flows into the nasal cavity through the nasolacrimal canal. If the channel is impassable – the lacrimation process is disrupted. This contributes to the accumulation of secretions in the lacrimal sac, further infection of the lacrimal sac is likely, which leads to the development of dacryocystitis. What factors contribute to inflammation of the lacrimal sac? What are the symptoms of dacryocystitis?
Classification and distribution of dacryocystitis. Who is more prone to dacryocystitis?
Dacryocystitis is classified by cause and course. According to clinical forms, dacryocystitis is acute, chronic and dacryocystitis of newborns. The etiology of dacryocystitis can be chlamydial, viral, bacterial, post-traumatic and parasitic.
Inflammation of the lacrimal sac, or dacryocystitis, occurs in approximately 7% of cases of ophthalmic pathology. Due to the narrow structure of the anatomical canal, women develop dacryocystitis 8 times more often than men. Usually, inflammation of the lacrimal sac affects the age group from 30 to 60 years, dacryocystitis of newborns is distinguished in a separate group.
Factors contributing to the development of dacryocystitis:
- sudden temperature changes;
- diabetes mellitus;
- presence of occupational hazards at work;
- a sharp decrease in immunity.
Causes of dacryocystitis development. When does the probability of the development of the process increase?
Any dacryocystitis develops against the background of obstruction of the nasolacrimal canal. If pathology is detected in newborns, this is due to congenital anomalies of the lacrimal ducts, the presence of a dense epithelial membrane in the lower part of the nasolacrimal canal, or the presence of an unresolved gelatinous plug. In adults, dacryocystitis appears against the background of tissue edema, which is pronounced in acute respiratory viral infections, sinusitis, rhinitis, adenoids and fractures of the bones of the nose, with damage to the lacrimal ducts and points as a result of injury to the eyelids.
When stagnant, tear fluid loses its antibacterial activity. This is accompanied by the multiplication of pathogenic microorganisms in the lacrimal sac. Therefore, the walls of the lacrimal sac gradually stretch, a sluggish inflammatory process develops inside. At the same time, the secret released from the lacrimal sac acquires a mucopurulent character.
Symptoms that indicate the development of acute dacryocystitis
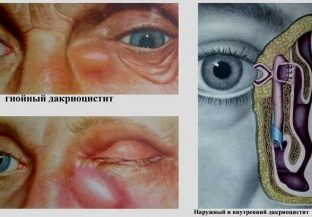
The clinical picture of dacryocystitis is very specific. The development of acute inflammation is characterized by vivid clinical symptoms. There is hyperemia of the skin and painful swelling in the projection of the inflamed lacrimal sac. There is marked swelling of the eyelids, narrowing or complete closure of the palpebral fissure. Redness may extend to the eyelids, cheeks, and bridge of the nose. Outwardly, it looks like erysipelas of the face, but with dacryocystitis there is no sharp delimitation of the focus of inflammation. Acute dacryocystitis is accompanied by jerking pains in the orbit, fever, chills, headache and other signs of intoxication.
A few days later, the infiltrate over the lacrimal sac softens, the skin becomes yellow, fluctuation appears. These symptoms indicate the development of an abscess, which can open on its own. Later, an internal or external fistula may form at this site, from which a tear or pus may be released. The spread of purulent cells to the surrounding tissue provokes the development of phlegmon of the orbit. In acute dacryocystitis, the recurrent nature of the course of the process is often observed.
Main clinical manifestations of chronic dacryocystitis
Chronic dacryocystitis is manifested by swelling in the projection of the lacrimal sac and constant lacrimation. Pressure on the swelling is accompanied by the release of a purulent or mucopurulent secret. The semilunar fold and conjunctiva of the eyelids are hyperemic. The long course of chronic dacryocystitis is accompanied by stretching of the lacrimal sac. The skin over the bag becomes thinner and takes on a bluish tint.
If dacryocystitis is diagnosed, urgent care should be sought to diagnose and treat dacryocystitis. Read our next article for diagnostic methods and treatment options for dacryocystitis.







Add a comment