The periorbital zone (“the area around the eyes”) is a complex of soft tissues surrounding the orbit, which are connected to its bony borders (points of fixation of muscles and connective tissue frame), as well as neurovascular bundles that provide blood supply and innervation to soft tissues.
Read on estet - portal . com , what Dr. Zoya Diwan tells about the vascular anatomy of the eyes and periorbital zone, knowledge of which is necessary to prevent vision loss after injection of fillers.
- The main arteries supplying blood to the eye and periorbital area
- What features of vascular anatomy must be taken into account when using fillers?
- Loss of vision after fillers: causes of complications
- Emergency assistance methods in case of complications after filler injection V
The main arteries that supply blood to the eyes and periorbital area
The main artery providing blood supply to the eye is the orbital artery (OA) . The location of the multiple branches of the GA varies from patient to patient.
For example, in 3% of people the GA arises from the middle meningeal artery, a branch of the external rather than the internal carotid artery.
The GA supplies blood to two distinct areas – the orbital (mainly the eye socket) and the periorbital (mainly the muscles and area around the eyes) – see Table 1 .
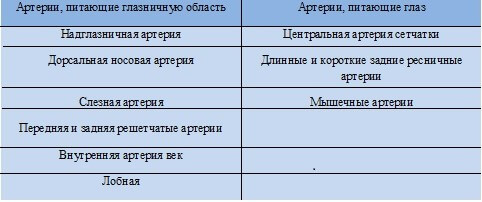
Table 1: Branches of the ophthalmic artery supplying the eye and orbital region
The internal carotid artery , as a rule, passes through the cavernous sinus and before leaving it forms a branch - the orbital artery , which enters the orbit through the optic foramen.
The external carotid artery has two branches that supply blood to the orbit: the infraorbital and middle meningeal arteries.
What features of vascular anatomy need to be taken into account when working with fillers?
Damage to some arteries when dermal fillers are injected is associated with an increased risk of complications.
Occlusion of the long and short posterior and anterior ciliary arteries can lead to symptoms of anterior ischemic optic neuropathy , including vision loss due to reduction or cessation of the ciliary blood supply, particularly to the optic nerve head, which these arteries supply.
Complications after Fillers: A Guide for Experts from Dr. Patrick Tracy
The supraorbital and dorsal nasal arteries are the terminal branches of the orbital artery; injection of filler into these arteries can lead to the formation of an embolus , which, with the reverse flow of blood, can move to any of the arteries that directly supply blood to the optic nerve or retina.
It is important to understand that there is a huge network of anastomoses between these arteries.
Diagram 1 shows the location of the main arteries that supply blood to the eye and orbit. All these arteries are branches of the ophthalmic artery. All branches of the ophthalmic artery and its anastomoses with other branches, as well as with the arterial branches of the external carotid artery (ECA) are depicted. These include branches of the ECA that anastomose with the branches of the internal carotid artery (ICA).
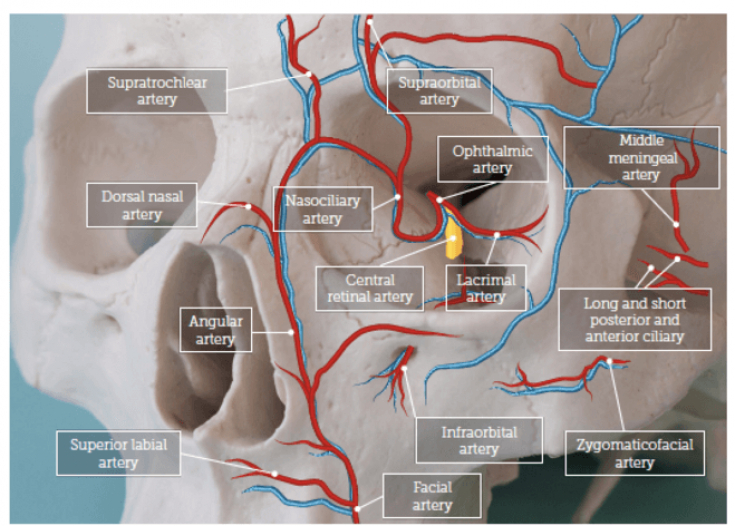
Diagram 1: Major arteries surrounding and supplying the orbit
|
|
For example, the infraorbital artery is a branch of the ECA and has anastomoses with branches of the ophthalmic artery (ICA branches), which are a potential route for the advancement of filler emboli and blockade of the ophthalmic artery or any of its branches.
Follow us on Instagram !
Another example is when the drug enters the angular artery during filler injection into the nasolabial fold. This may result in filler embolization of the dorsal nasal artery, which anastomoses with the angular artery and ultimately provides access to the GA.
The most dangerous area in the context of correction with fillers is the glabellar region - almost 40% of 98 recorded cases of vision loss occurred after injection of drugs into the glabellar region.
Under the pressure of the syringe, the filler passes through the HA and after the pressure stops, the systolic pressure in the HA pushes the embolus into the branches of the HA, including the central retinal artery, which can lead to loss of vision .
Thus, the risk of vision loss exists when dermal fillers are injected into almost any area of the face.
Loss of vision after fillers: causes of complications and actions in case of complications
Loss of vision usually occurs within a few seconds after the corresponding artery is damaged.
If the central retinal artery is affected, after an hour and a half, vision loss becomes irreversible ( according to the results of a study conducted by C. J. Hwang et al . in 2019).
However , S. Tobalem et al . in 2018, they reviewed the literature and found that the response time is significantly less - only 12-15 minutes.
Signs and symptoms of advancing vision loss may include:
- pain;
- sudden loss or blurred vision;
- ptosis and weakness/paralysis of the eye muscles (ophthalmoplegia).
The above symptoms occur due to impaired blood flow to multiple arteries surrounding the eye, including the supra- and infraorbital.
Recommendations for cosmetologists: Dublin protocol for the treatment of complications
According to the results of a meta-analysis conducted in 2015 by Dr. K. Beleznay , a total of 98 cases of vision loss were recorded after injections of fillers (including autologous fat, hyaluronic acid, poly-L-lactic acid and calcium hydroxyapatite.
In 38 out of 98 cases, vision loss occurred after the injection of fillers into the area between the eyebrows ; Also, the most dangerous areas in the context of this complication are the areas of the nose, nasolabial fold and forehead.
There is a risk of vision loss when dermal fillers are injected into almost any area of the face.
As for drugs , in almost 50% of cases, patients were injected with autologous fat, in 23.5% with hyaluronic acid, the remaining cases were poly-L-lactic acid, paraffin, polymethyl methacrylate, silicone oil and calcium hydroxyapatite.
In 11 out of 98 cases, a complication occurred during correction of the periorbital zone (including the nasolacrimal groove and cheeks).
In most cases, vision, unfortunately, could not be restored. Complications from the nervous system were recorded in 23.5% of cases.
In 2019, the authors conducted a similar study that identified 48 new cases of partial or complete vision loss after filler injections from January 2015 to September 2018.
In 81.3% of cases, complications occurred after the injection of HA fillers. In 10 cases, complete restoration of vision was reported, in eight – partial restoration.
Methods of emergency assistance in case of complications after injection of fillers
Early interventions, including hyaluronidase injections and massage of the affected area , have been shown to be effective in restoring full or partial circulation to the eye area in some patients.
Prevention and treatment of complications of aesthetic correction in the periocular area
Walker and King have compiled a list of actions that a practitioner should take if this complication occurs:
- If the patient complains of eye pain or sudden loss of vision, the procedure should be stopped immediately.
- Place the patient in a supine position.
- Contact an ophthalmologist.
- Before the ophthalmologist arrives, reduce intraocular pressure with 1-2 drops of 0.5% timolol , allow the patient to breathe into a paper bag and 300 mg of aspirin .
- Try to eliminate the embolus by massaging the eye .
- Inject a dose of hyaluronidase into the treated area (retrobulbar injections are performed only by an ophthalmologist for 90 minutes).
In addition to the above steps, the Aesthetics Interventional Induced Visual Loss (AIIVL) Consensus Group recommends sublingual glyceryl nitrate spray.
Based on materials from Aesthetics magazine.







Add a comment