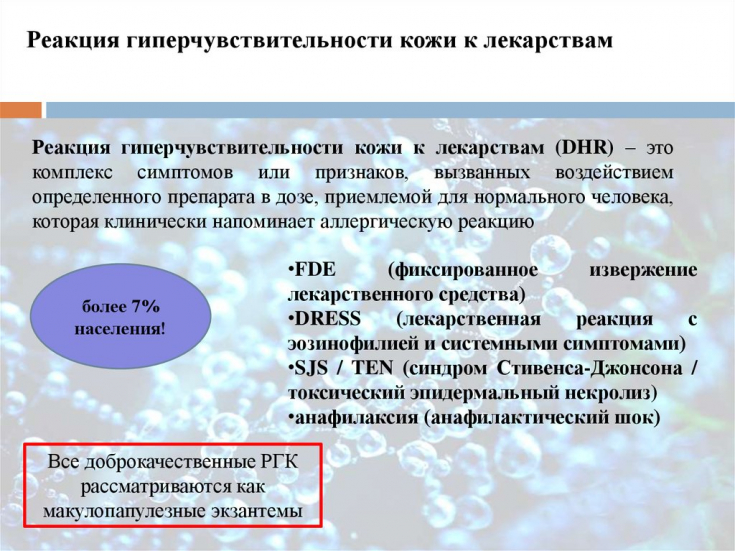
Common drug reactions account for 90% of all toxic skin reactions in the practice of a dermatologist. They appear from the 4th to the 14th day after the start of a new treatment and even on the 1st-2nd day of stopping.
Often such a clinic is assessed as erythema multiforme exudative (EEE). It should be emphasized that the discussion on the assessment of BEE as the first stage of further transformation of the process into Stevens-Johnson syndrome is still ongoing.
Find out in the article on estet-portal.com about the main causes of toxic skin reactions in the practice of a dermatologist and the main approaches to the treatment of this pathology.
Clinical picture of toxic skin reactions
The danger of toxic skin reactions lies in the fact that urticaria and angioedema can be combined in 50% of cases, and in 80-100 cases (per 1 million patients with this diagnosis) are accompanied by anaphylaxis.
Follow us on Instagram!
Acute generalized eczematous pustulosis is characterized by fever and a pustular rash. Clinically, skin reactions (mainly on the face and hands) are observed in the form of non-follicular pustules against the background of erythema and edema. In more severe cases, patients note the presence of purpura, vesicles, blisters, rashes on the mucous membranes. Toxic skin reactions usually appear 2 days after taking the medication, and disappear spontaneously after 15 days.
According to the observations of dermatologists, purpuric rashes have become more frequent with a fairly frequent prescription of anticoagulants.
Severe toxic skin reactions in the practice of a dermatologist
Drug skin reaction with eosinophilia and systemic symptoms (DRESS syndrome) occurs in 1 in 10,000 drug use cases and has a mortality rate of 10%. Clinical manifestations begin 2-6 weeks after the first use of the agent, which has become a specific trigger factor. Severe polymorphic skin reactions (erythema, urticaria, hemorrhages, blisters) are clinically fixed. Visceral disorders are varied and severe: hepatitis, arthralgia, pulmonary infiltrates, nephritis.
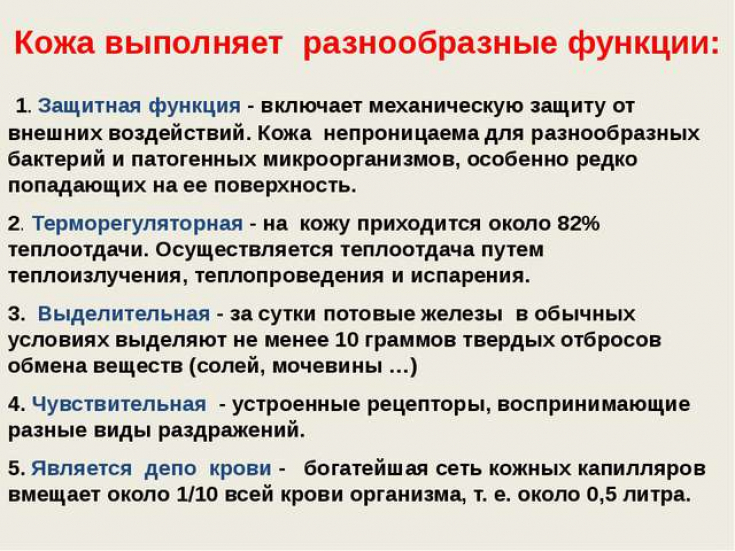
Immune function of the skin to guard the health and order of the body
Among the toxic skin reactions in the practice of a dermatologist, fixed toxic rashes are most often observed. Clinically noted: erythematous plaques (maybe in the center of the bubble), possible damage to the mucous membranes (lips, genitals), after a few days, post-inflammatory pigmentation remains; characterized by the absence of erosion on the mucous membranes. Basically, such toxic skin reactions develop after barbiturates, tetracyclines, sulfonamides.
Stevens-Johnson Syndrome – severe pathology in the practice of a dermatologist, which requires emergency care, in which small blisters appear on purple spots, usually on the trunk (sometimes up to 10% of the body surface is affected). In the case of toxic epidermal necrolysis, the same reactions of the skin with wheals merging where the leading sign − Nikolsky symptom with rejection > 30% of the skin surface.
Five skin manifestations that can save lives if diagnosed
Chronic skin reactions in the practice of a dermatologist
In addition to acute skin reactions, a dermatologist may experience chronic toxic skin manifestations. Diagnostic signs of chronic skin reactions can be pigmentary changes, drug-induced pemphigus, drug-induced bullous pemphigoid, drug-induced lupus erythematosus, pseudolymphoma, acneiform rashes.
Approaches to the treatment of toxic skin reactions
It is in the treatment of drug-induced toxic skin reactions that preference is given to different options for detoxification. The syndrome of endogenous intoxication is involved in the formation of the clinical picture of various toxic reactions of the skin and almost always contributes to the implementation of toxicoderma. Among the large group of hepatoprotectors, amino acid preparations (betaine, arginine, ornithine, glutamine, methionine) are relevant, which have a comprehensive therapeutic effect and are characterized by cytoprotective, detoxifying, angioprotective and antioxidant properties.
Allergy to Latex – who is at risk of a pathological reaction to an allergen
The pharmacodynamic features of hepatoprotectors and detoxification agents justify their prescription by dermatologists in case of mild to moderate toxic skin reactions.
Severe forms of toxic skin reactions, such as Stevenson-Johnson syndrome, require the appointment of glucocorticosteroid drugs, infusion therapy, as well as active external therapy: removal of necrotic epidermis, topical use of antiseptic solutions by a dermatologist. Often, the treatment of severe forms of toxic skin reactions is carried out by a dermatologist together with an intensive care doctor, a surgeon, an ophthalmologist and, if necessary, a pediatrician.
What a dermatologist should know about hives in children
Another side of preventing the development of toxic skin reactions is such a treatment feature as the possibility of widespread use of topical therapy. This approach is facilitated by the appearance of a number of drugs in which the molecules of systemic drugs are introduced into dosage forms for external use. The active substance of such medicines can enter the dermis and skin appendages.
So, the following approaches to overcoming toxic drug-induced skin reactions can be distinguished: exclusion of polypharmacy, timely diagnosis of toxic drug-induced reactions, prescription of hepatoprotectors, exclusion of systemic drugs by replacing them with topical ones.
A new antibiotic in the treatment of pyoderma







Add a comment