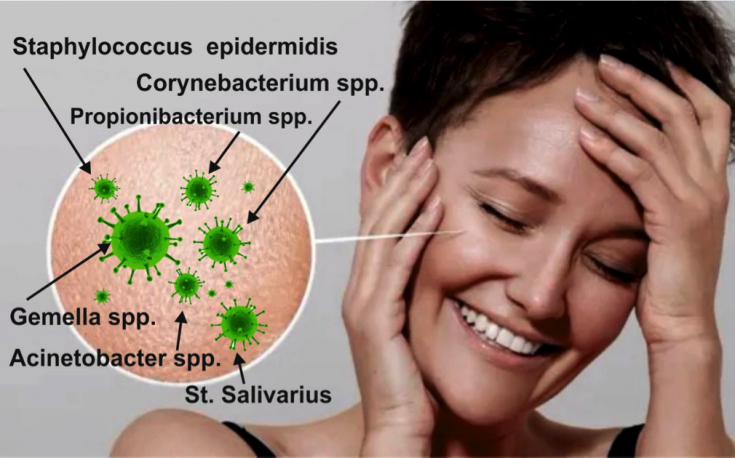
The search for antibacterial agents, the use of which would be effective in the treatment of infections caused by resistant microflora, remains one of the pressing issues of public health throughout the world. One of the currently known ways to obtain antimicrobial agents is the result of the extraction of specialized metabolites of certain bacteria, especially members of the Actinomycetes family. Methicillin-resistant Staphylococcus aureus (MRSA) — it is a resistant to certain antibiotics species of staphylococcus aureus. MRSA can cause various diseases, in particular, skin and subcutaneous tissue lesions.
Find out in the article on estet-portal.com about the results of a study on the effectiveness of new generation antibacterial drugs in the treatment of resistant staphylococcal flora.
- A new way to obtain antibacterial drugs
- The mechanism of action of new generation antibacterial drugs
- Practical significance of antibacterial preparations of a new class
A new way to obtain antibacterial drugs
Over time, a single platform approach to screen for actinomycete activity has shown a progressive decline in drug efficacy.
Subscribe to our page on Instagram!
But a new method has appeared - sequencing of the bacterial genome, which allows to identify previously unknown biosynthetic gene clusters. However, the prediction and synthesis of therapeutically significant bioactive compounds based on the screening of gene clusters, first of all, requires specification of search priorities.
Beware of the fungus! How and why does dermatophytosis infection occur? In a recent study, scientists from McMaster University, Canada, presented a new group of antibacterial drugs
that have a unique mechanism of action against bacterial flora: by blocking the functions of the cell wall of these microorganisms.
methicillin-resistant
Staphylococcus aureus (MRSA), which according to studies may be present in 7-30% of lesions of the skin and subcutaneous tissue. The mechanism of action of new generation antibacterial drugs
In the course of the study, in order to predict the divergence of the pathways for the synthesis of glycopeptide antibacterial drugs, the authors relied on the phylogenetic patterns of bacterial gene biosynthesis in the absence of resistance determinants known to them. In particular, when studying individual members of the glycopeptide group, the researchers focused on the genome of thosethat had no known mechanisms of resistance
, anticipating the presence of a potential unknown antibacterial effect.
Such conditions made it possible to predict the synthesis of new antibacterial drugs.
Using this approach, scientists have identified two potential representatives of the functional class of glycopeptides that differ in their original mechanism of action. In particular, it has been shown that, by binding to peptidoglycans,
complestatin and corbomycinblock the activity of autolysins ─ essential peptidoglycan enzymes that are involved in cell wall remodeling processes in the bacterial growth phase.
Why does the skin itch: features of the diagnosis and treatment of itching
It has been established that corbomycin and complestatin are characterized by a low level of development of resistance
, as well as sufficient antibacterial efficacy when used in laboratory conditions with simulatedskin infection caused by methicillin resistant aureus staphylococcus. Practical significance of new class of antibacterial drugs
Commenting on the results of the study, the authors focused on the fact that the mechanism of action of the presented antibacterial drugs, like other individual antibiotics, is associated with an effect on the bacterial cell wall. At the same time, for example, unlike representatives of the penicillin group, which prevent the synthesis of the cell wall, new antimicrobial compounds, on the contrary, block its destruction
. The result is that under such circumstances the growth of the bacterial cell is excluded.How does the activity of phagocytes change in acneMore useful information on our YouTube







Add a comment