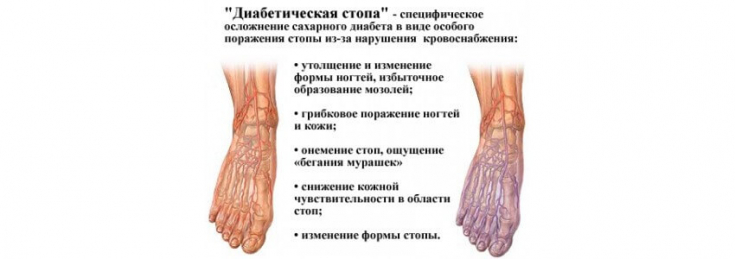
Diabetic Foot Syndrome (DFS) − a specific symptom complex of foot lesions in diabetes mellitus (DM), the basis of the pathogenesis of which is diabetic micro-, macroangiopathy, peripheral neuropathy of the lower extremities and osteoarthropathy.
These processes develop in parallel, mutually burdening each other, with the addition of severe purulent-necrotic lesions, which are characterized by a special composition of the microflora and a course against the background of deep metabolic disorders and immunosuppression.
Find out in the article on estet-portal.com about the latest recommendations regarding the diagnosis and treatment of patients with diabetic foot syndrome.
- Assessing the risk of developing diabetic foot syndrome
- Frequency of diabetic foot syndrome risk assessment
- Measures that are prohibited in the treatment of diabetic Assessing the risk of developing diabetic foot syndrome When examining a patient with diabetes, it is recommended to remove shoes, socks, bandages and examine both feet for the presence of such risk factors for developing diabetic foot: neuropathy;
lower limb ischemia;
ulcers; corns;
- presence of inflammation, deformity;
- gangrene;
- Charcot arthropathy.
- Follow us on
annual ankle-brachial index to assess the state of the peripheral arteries. Individuals with diabetes may have false positive results due to arterial calcification.
Diabetes mellitus in young patients: features of managementTo assess the risk of developing diabetic foot syndrome in the clinic, it is recommended to use the following risk stratification:
1. Low risk: no risk factors except callus;
2. Moderate risk: Presence of deformity, neuropathy, or signs of limb ischemia.
3. High Risk:
history of ulcer or amputation; patient receiving renal replacement therapy;
combination of neuropathy and non-critical limb ischemia; combination of neuropathy with callus and/or deformity
- ;
- Combination of non-critical limb ischemia with callus and/or deformity.
- Frequency of risk assessment for diabetic foot syndrome
- Recommended intervals for assessing the risk of developing DFS:
- Annually for low-risk individuals;
Every 3-6 months for those at moderate risk;
Every 1-2 months for high-risk individuals; Every 1-2 weeks for high-risk and critically ill patients.
The
threatening conditions in the presence of diabetic foot syndrome
ulcer with existing limb ischemia;
gangrene of the foot or individual fingers.
- Development of new forms of insulin preparations for the treatment of diabetes mellitus
- If the patient has an ulcer, the physician should evaluate and record the data in the medical history. It is recommended to use a standardized system for documenting the severity of a foot ulcer
SINBAD (Site, Ischaemia, Neuropathy, Bacterial Infection, Area and Depth).
Measures that are prohibited in the treatment of diabetic footDue to possible complications, it is not recommended to use the following methods: in the treatment of diabetic foot syndrome
electrostimulation therapy;
platelet-rich plasma (PRP therapy); dalteparin and regenerative matrices; growth factors (G-CSF, EGF, PDGF, TGF-.beta.);
- hyperbaric oxygen therapy.
- If there is a suspicion of an infection in a diabetic foot, it is recommended to take a tissue / bone sample and send it for microbiological analysis.
- It is recommended to x-ray the affected foot(s)
- of the patient to determine the extent of the lesion. In the presence of an infection of a diabetic ulcer, it is necessary to rule out osteomyelitis
- .
start antibiotic therapy as soon as possible in patients with DFS. It is recommended to start the 1st line of therapy with oral forms of antibacterial drugs, if the severity of the condition does not require a parenteral form of administration.
When prescribing parenteral (intravenous) antibiotic therapy, it is recommended to evaluate after 48 hours and if the patient's condition improves − switch to oral form.
It must also be remembered that a foot or ankle fracture in a person with diabetes can lead to
Charcot's arthropathy
 This pathology can be suspected in the presence of redness, localized fever, edema, or deformity (particularly when the skin remains unchanged), especially in the presence of peripheral neuropathy or renal failure.
This pathology can be suspected in the presence of redness, localized fever, edema, or deformity (particularly when the skin remains unchanged), especially in the presence of peripheral neuropathy or renal failure.
radiography of the affected foot and ankle
is performed. If the x-ray shows no changes, it is recommended toperform an MRI.
Drug therapy for diabetic complicationsAs a treatment for this pathology, a non-removable individual unloading bandage
can be used. If a bandage is not appropriate in the treatment of the patient, it is recommended that aremovable unloading bandage be considered. However,, bisphosphonates are prohibited for the treatment of patients with acute Charcot arthropathy.
Patients who have deformity due to previous Charcot arthropathy are at high risk of developing an ulcer.Follow our news on YouTube channel:







Add a comment