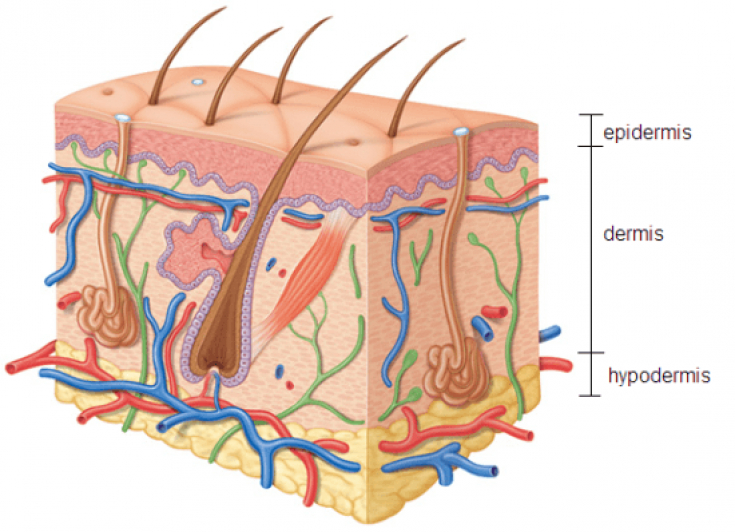
Toxicoderma – acute inflammatory lesions of the skin, sometimes also mucous membranes, as a reaction to substances circulating in the blood that have a sensitizing, toxic, dysmetabolic effect. A distinctive factor from dermatitis is the penetration of the allergen into the skin by the hematogenous route.
The toxic-allergic agent can enter the blood in several ways: through the respiratory tract, the gastrointestinal tract, through the skin, or even synthesized in the body.
Direct contact of the surface layer of the skin with the allergen, at the site of the lesion, does not always occur. A toxic-allergic agent can enter the body both by ingestion of food or drugs, and by inhalation. Further, the allergen spreads in the body through the circulatory system and affects the skin already "from the inside"; organism, read more in the material estet-portal.com.
Toxicoderma: the etiology of the disease
Drug toxicoderma mainly develops when taking antibiotics, sulfonamides, vitamins, rivanol, the use of novocaine, furacilin, gamma globulins, blood serum products.
Food products can also contain toxic-allergic agents. These can be preservatives, dyes, flavors contained in the products. They are the most common causes of the disease.
«Food allergens– the most common cause of toxicoderma in general.
It is also worth considering the possibility of a person having idiosyncrasy – individual intolerance to any substance.
Follow us on Instagram
Of the professional factors in the development of toxicoderma, it is worth noting the effect of substances containing chlorine, nickel, cobalt, and iodine in their structure.
Don't forget about possible autointoxication. It occurs due to the accumulation of non-typical metabolic products and is caused by a metabolic disorder or a violation of their excretion from the body.
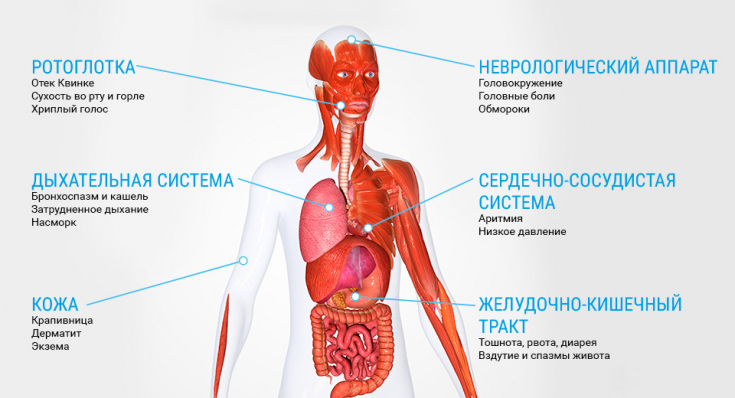
Routes of allergen entry:
1. injection
2. alimentary
3. inhalation
4. transdermal
5. endogenous toxins
Fig. 1 Correlation of etiological factors.
The mechanism of development of toxicoderma includes two components:
• allergic − one of the four types of reaction (anaphylactic, cytotoxic, immunocomplex, cell-mediated);
• toxic – pseudo-allergies, drug side effects, metabolic disorders.
Risk factors, according to studies, are smoking, frequent stress, the use of low-quality products or those containing a large number of additives.
Clinical picture of toxicoderma
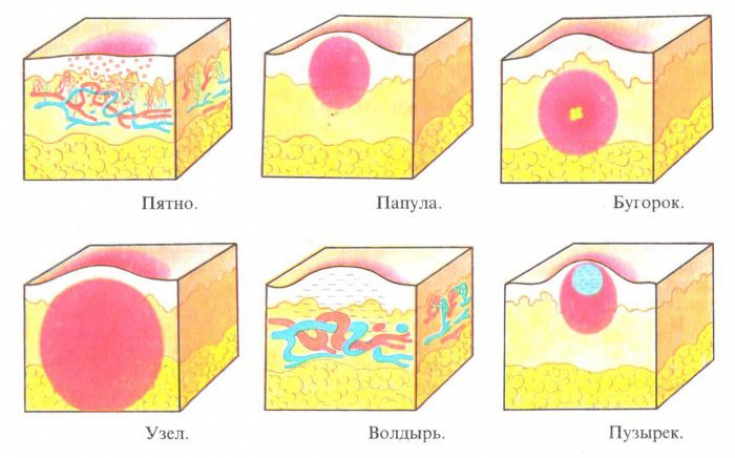
Clinical manifestations of toxicoderma can be very diverse. The main symptom is an inflammatory lesion of the skin, which can manifest itself in the form of rashes of the following nature: erythematous spots, urticarial, papular, pustular, bullous, nodular and vesicular rash.
Read also: Five skin manifestations requiring urgent diagnosis and treatment
In some cases, the clinical picture is similar to common dermatological diseases and infections accompanied by skin lesions: scarlet fever, erythema intermittent, lichen rosea, measles, etc. Clinical manifestations may have an acute onset, accompanied by a violation of the general condition of the body:
• rising temperature
• malaise
• swollen lymph nodes
• nausea
• vomit
• arthralgias
• myalgias
"Due to the variability of clinical manifestations, be careful not to confuse toxicoderma with other diseases."
Due to the polymorphism of the manifestations of the disease, it is imperative to conduct a differential diagnosis with common dermatological and infectious diseases that have skin manifestations.
What are the classifications of toxicoderma
The most common classifications used by physicians are by severity and by prevalence (volume of injury).
Severity:
• mild
Accompanied by itching, the most frequent manifestations – erythematous spots, urticarial and papular rashes. Symptoms disappear after a few days, after the cessation of the intake of the toxic-allergic agent into the body.
• moderate
Of the symptoms present: rashes, itching of the skin, subfebrile condition is possible. The nature of the rash: urticaria, solitary blisters, widespread erythema, vesicles, nodules. In the general blood test, the following can be detected: eosinophilia, increased ESR.
• severe
Characterized by a significant rise in temperature (up to 40 ° C), nausea, vomiting. May present with urticaria and Quincke's edema, generalized rashes and be accompanied by anaphylactic shock. Severe toxicoderma also includes Lyell's syndrome, Stevens-Johnson syndrome. In the general blood test, more pronounced changes are already observed: an increase in eosinophilia and an increase in ESR.
See also: Severe and rare forms of toxic-allergic dermatitis
Classification by prevalence:
1. limited (the number of elements is not significant, they do not merge, the diameter of the rashes is less than 3 cm)
2. common (there are confluent elements, the diameter of the rash is more than 3 cm)
Diagnosis of toxicoderma is based on the clinical picture, a thorough examination of the patient, a detailed history of the disease, the results of laboratory and instrumental studies (not specific in this case), the exclusion of pathologies similar in manifestations other etiology.
The main directions in the treatment of toxicoderma
First of all, assistance is aimed at stopping the entry of a toxic-allergic agent into the body, removing it from the body and stopping symptoms.
For mild to moderate severity, outpatient treatment is possible. As a rule, in these cases, detoxification, desensitizing and symptomatic therapy is carried out. If the source of the toxin is removed, recovery occurs in a few days.
"The main stage of treatment – exclude further entry of the toxic-allergic agent into the body.
In cases where there are signs of: severe intoxication, fever, extensive skin lesions, impaired consciousness, shortness of breath, tachycardia – hospitalization, the use of systemic hormonal drugs, intravenous antihistamines and more intensive methods of detoxification are necessary. In extremely severe cases, hospitalization in the intensive care unit may be necessary.
The main groups of drugs used in the treatment of toxicoderma: antihistamines, systemic and / or local corticosteroids, sorbents. If the affected areas of the skin are infected with bacteria or fungal flora – prescribe appropriate antibiotics and antifungals.
"One of the most frequent complications of toxicoderma – secondary infection.
In the most difficult cases, a plasmapheresis procedure can be performed to detoxify.
Read dermatology news on Facebook
In order to prevent toxicoderma, it is necessary to avoid or minimize the use of drugs that most often cause this disease. Patients with a tendency to allergic reactions should be explained how important it is to watch what foods they eat.







Add a comment