Today, secondary syphilis is much less common than before, but it is syphilis in the secondary period that is the most difficult to diagnose.
The disease can occur under the guise of psoriasis, versicolor, toxicoderma, trichomycosis and even tonsillitis.
Knowing the clinical differences between secondary syphilis and other skin and infectious diseases will help to establish the diagnosis in time and carry out specific treatment.
On estet-portal.com read about the main clinical criteria for secondary syphilis, as well as about the diseases with which secondary syphilis must be differentiated.
"Roller coaster": features of the course of secondary syphilis
Secondary syphilis develops after the appearance of a hard chancre within 6-8 weeks. The secondary period is characterized by an undulating course and a generalized spread of treponema with the development of infectious immunity and allergies in response.
There are fresh and recurrent periods of secondary syphilis, successively replacing each other for 2-5 years.
After each recurrence, the rashes decrease in number and become less pronounced.
Also, some patients experience changes in skin pigmentation and alopecia.
Follow us on Facebook
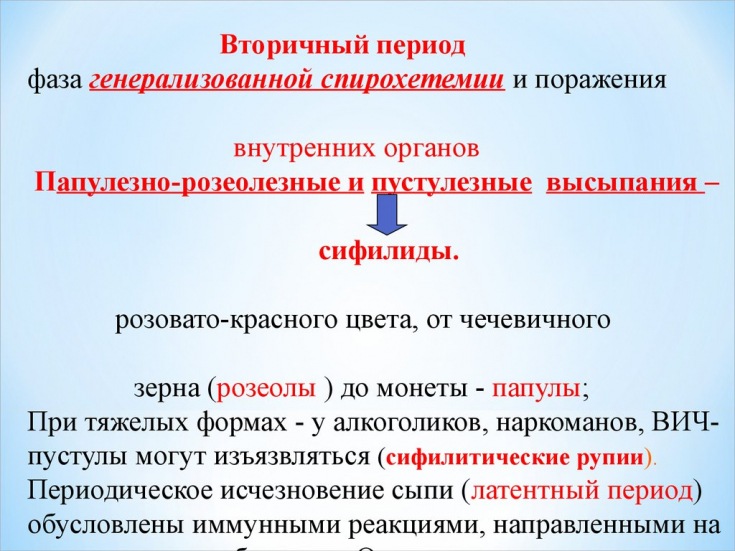
The beginning of the secondary period of syphilis is characterized by the appearance of a polymorphic rash in the form of roseola, papules or pustules due to endogenous intoxication.
Main features of the secondary period:
• Multiple rashes on the skin and mucous membranes that do not merge and pass without a trace;• as a rule, the patient has no subjective sensations;
• serological tests are 99.9% positive;
• the color of secondary syphilides is copper-red and eventually becomes a stagnant brown color;
• rash tends to resolve spontaneously without treatment;
• no acute inflammation;
• high contagiousness of secondary syphilides, especially if erosions and ulcers form;
• rapid disappearance of secondary syphilides after specific therapy.
Location in the folds of the skin or around natural openings, syphilides can change their shape (appearance of vegetation, weeping, erosion).
In search of the causative agent of syphilis: a mysterious disease
For secondary syphilis, a polymorphism of rashes is characteristic, while each syphilis has its own varieties.
The most common forms of syphilides – macular and papular:
1. Spotted syphilide must be differentiated from toxicoderma, pink lichen, marbled skin, childhood infectious diseases, typhoid fever and spots after a lice bite;2. Papular syphilide has similarities with guttate parapsoriasis, lichen planus, psoriasis vulgaris and molluscum contagiosum;
3. Vegetating papules (condylomas lata) with acute warts, vegetative pemphigus and soft chancre;
4. Papular syphilis of the palms and soles may resemble a clinic of psoriasis or eczema with the same localization.
Read also: Typical and atypical signs of syphilis: how to recognize the disease in time
Also, the erosive form of papular syphilis must be differentiated from interdigital epidermophytosis of the feet – a fairly common skin disease of a fungal nature.

Other forms of syphilis are less common, but can simulate the clinical picture of well-known diseases.
Pustular syphilis must be distinguished from impetigo vulgaris, sycosis and acne vulgaris, and ecthyma vulgaris.
Syphilitic angina can simulate the clinic of catarrhal and ulcerative necrotic angina, and with the formation of a chancre – traumatic ulcer or chancriform pyoderma.
For the differential diagnosis of secondary syphilis, the collection of anamnesis, serological reactions, specific manifestations and the characteristic undulating course of the disease are of great importance.
The sooner the diagnosis is made, the greater the chance of a successful cure of the patient and preventing infection of others.
Thank you for staying with estet-portal.com. Read other interesting articles in the "Venerology" section. You may also be interested in:
What are the basic principles of syphilis treatment







Add a comment