Herpetic infection can be a breeding ground for a fruitless marriage, as the viruses have an adverse effect on the reproductive health of both women and men. But even during pregnancy, herpes viruses cause a serious risk of intrauterine infection of the fetus and adverse pregnancy outcomes [1, 4, 5, 7]. Herpes simplex virus (HSV) is often the cause of neurological, somatic and endocrine problems in newborns and older children [3]. Particularly dangerous is the genital localization of herpes, which occurs in pregnant women in 7–35% of cases [2, 6].
The purpose of this work was to study the optimization of the diagnosis of herpes infection in pregnant women with a burdened obstetric and gynecological history (OAGA) in the dynamics of pregnancy.
74 multiparous women were examined: 49 nulliparous and 25 multiparous. The age of the patients ranged from 20 to 41 years. All women had OAHA, and they were referred to MONIIAG with a diagnosis of "chronic herpes virus infection";. The study was conducted in dynamics, starting from 16–24 weeks. pregnancy.
Virological (rapid culture method - RCM), molecular biological (PCR, real-time PCR) and serological (ELISA) methods were used to detect HSV markers. Blood, urine and urogenital scrapings were studied as clinical material from pregnant women. The viral load in various clinical materials was judged by the amount of HSV DNA, which was determined by PCR-rt. For each sample, the value of the threshold cycle Ct (threshold cycle is the point at which fluorescence exceeds the background value) was recorded and the medians were calculated. The obtained values of the threshold cycle (Ct) were compared with the values of standard control samples with a known content of DNA in the sample. To assess the parameters of the humoral response, blood sera were examined by ELISA for the presence of specific antibodies to HSV (AT) of the IgM and IgG classes.
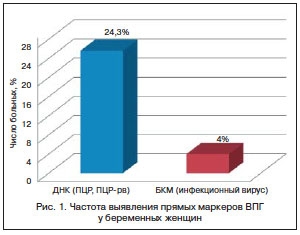
Among the examined pregnant women, a high infection rate was noted: in 43 (58%) of 74 women, one or another urogenital infection (UGI) of viral and/or bacterial etiology was detected. The method for diagnosing UGI is PCR with a qualitative assessment of the result. A detailed study of the anamnesis revealed that mixed UGI was detected in 21 (28%) pregnant women. The infection structure included a whole range of UGI pathogens: Ureaplasma urealiticum, Micoplasma hominis, Toxoplasma gondii, Gardnerella vaginalis, Chlamidia trahomatis, Candida albicans, Human papillomavirus. In 22 (30%) pregnant women, the only causative agent of UGI was found: Ureaplasma urealiticum - in 15 (20.4%), Micoplasma hominis - in 4 (5.4%). At the same time, the patients did not complain, there were no clinical signs of infection.At the first stage of the examination of patients, a comparative analysis of the frequency of detection of direct markers of HSV (infectious activity of the virus and HSV DNA) was carried out. None of these women had any clinical manifestations of genital herpes during the examination. The patient was considered infected if the virus marker was found in at least one studied clinical material. During the entire examination period, HSV markers were detected in 18 (24.3%) pregnant women. At the same time, HSV DNA was detected in 15 (20.3%) pregnant women, infectious virus - in 3 (4%) women (Fig. 1). Differences in detection rate of HSV DNA compared to infectious virus were statistically significant (p<0.05).
 The frequency of HSV detection in different clinical materials was determined. 525 biological materials from pregnant women were examined for the presence of direct markers of HSV: 175 samples of blood, urine and urogenital scrapings each. When analyzing all the studied samples in total by all the methods used (BCM, PCR and PCR-rt), most often HSV markers were detected in urogenital scrapings (27/175, 15.4%) and urine samples (20/175, 11.4%) , significantly less frequently in the blood (4/175, 2.3%, p<0.05).
The frequency of HSV detection in different clinical materials was determined. 525 biological materials from pregnant women were examined for the presence of direct markers of HSV: 175 samples of blood, urine and urogenital scrapings each. When analyzing all the studied samples in total by all the methods used (BCM, PCR and PCR-rt), most often HSV markers were detected in urogenital scrapings (27/175, 15.4%) and urine samples (20/175, 11.4%) , significantly less frequently in the blood (4/175, 2.3%, p<0.05).
Along with the total assessment, a comparative analysis of the frequency of detection of HSV markers depending on the method was carried out. HSV DNA was detected by PCR in 16/525 (3%) samples, by PCR-rt - in 30/525 (5.7%) samples. Statistical analysis showed that the PCR-rt method detected viral DNA significantly more often than the classical PCR method (p<0.05). Infectiously active virus in biological materials (BCM) was detected much less frequently than HSV DNA - in 5/525 (1%) samples. Thus, the sensitivity of detection of HSV by the PCR-rt method exceeded that of the other two methods used.
The low detection rate of HSV by BCM in clinical samples can be explained either by the absence of an infectious virus in these samples in the presence of viral DNA, or by the lower sensitivity of the BCM than by PCR.
Studies have shown that the amount of DNA found in urine and urogenital scrapings is higher than the amount of DNA in blood samples. Statistical processing of the cycle threshold (Ct) values proved to be statistically significant (p<0.05).
Analysis of blood sera showed that 64/74 (86.5%) pregnant women had anti-HSV-IgG antibodies at the initial examination. Anti-HSV-IgG antibodies were absent in 10 (13.5%) women. In 2 (2.7%) pregnant women, during the initial examination, in addition to IgG-AT, antibodies of the IgM class were detected, which are markers of the acute phase of infection.
When assessing the avidity of IgG-Ab, it was found that in all 64 (86.5%) women who had IgG-Ab to HSV, antibodies were characterized by high avidity (AI > 50).
Pregnant women were examined in dynamics at three stages of pregnancy: in the second and third trimesters and before childbirth. During the initial examination in the second trimester of pregnancy, HSV markers were detected in 12 (14.8%) women by BCM and/or PCR methods. In 8 (12.2%) pregnant women, the detection of HSV markers was combined with the detection of highly avid IgG antibodies (AI > 50) with high titers (1:320). Of the examined pregnant women, IgG-ATs were not detected in two, which indicates primary infection.
Change in the concentration of IgG-AT or detection of antibodies with high titers in blood serum during the study in dynamics was accompanied by the detection of direct markers of HSV during the entire examination in 3 pregnant women. In one pregnant woman, IgG-AT were not detected, despite the detection of HSV markers throughout the study.
In 2 (3%) women, direct markers of HSV were detected during the initial examination in combination with IgM-AT. One of these women had a pregnancy that ended in a miscarriage in the second trimester.
In the third trimester of pregnancy, HSV markers were detected for the first time in 3 out of 74 pregnant women. A serological study showed that one woman had no antibodies to HSV. Upon further examination of this pregnant woman, the appearance of low avid (AI < 50) IgG antibodies with low titers of 1:20 was observed. This indicated primary infection. Reactivation of the infection occurred in 2 patients, while one had highly avid IgG-ATs with high titers of 1:320, the other had an antibody titer of 1:20.
The last examination of women before childbirth showed that HSV markers were detected for the first time in 3 pregnant women, despite the presence of antibodies to HSV, which indicated reactivation of the herpes infection.
In 4 (5.4%) pregnant women, HSV markers were detected throughout the entire examination. When analyzing the viral load in clinical samples, it was found that in 2 pregnant women, the viral load increased in dynamics with increasing gestational age: from 100 cDNA/ml at the initial examination to 10,000 cDNA/ml at the last examination period. The other two showed no change in viral load.
Thus, according to the results obtained, starting from the second trimester of gestation, 15 (20.3%) of 74 pregnant women experienced reactivation of herpes virus infection. Primary infection was diagnosed in 3 (4.0%) pregnant women, and 2 (2.7%) patients were infected in the second trimester of pregnancy and 1 (1.3%) in the third. Asymptomatic carriage was revealed in 49 (66.2%) pregnant women. In 7 (9.5%) women referred to MORIAG with a diagnosis of chronic HSV infection, HSV infection was absent throughout pregnancy (Fig. 2).
 A serological examination of 74 pregnant women over time showed that reactivation of a herpes infection is not always accompanied by the detection of high titers of IgG-AT or an increase in titers over time. So, in 3 out of 15 (40%) women with HSV reactivation, IgG-AT titers with low values (from 1:20 to 1:80) were detected.
A serological examination of 74 pregnant women over time showed that reactivation of a herpes infection is not always accompanied by the detection of high titers of IgG-AT or an increase in titers over time. So, in 3 out of 15 (40%) women with HSV reactivation, IgG-AT titers with low values (from 1:20 to 1:80) were detected.
The frequency of detection of markers of herpes infection in pregnant women depends on the diagnostic methods used (virological, molecular biological, serological) and the diagnostic media studied (blood, urine, urogenital scrapings). Molecular biological methods (PCR, PCR-rt) have the greatest diagnostic value in the study of material from media such as urine and urogenital scrapings.
Reactivation of a herpes infection is not always accompanied by the detection of high titers of IgG-AT or an increase in titers over time. This indicates the low ability of the immune system of a pregnant woman to produce a sufficient amount of antibodies even in the presence of direct markers of HSV and proves the need for immunocorrective measures in pregnant women with a high infectious risk.
According to www.rmj.ru/
LiteratureMakatsaria A.D., Bitsadze V.O., Akinshina S.V. Systemic inflammatory response syndrome in obstetrics. M.: Med. inform. agency. 2006. S. 448.
- Nikonov A.P., Astsaturova O.R. Genital herpes and pregnancy // Gynecology. 2002. V. 4. No. 1. S. 4–6.
- Poletaev A.V., Budykina T.S., Morozov S.G. Maternal infection as a cause of fetal and newborn pathology // Allergology and Immunology. 2001. Vol. 2. No. 2. P. 110–116.
- Tsinzerling A.V., Melnikova V.F. Perinatal infection: a practical guide // Praktich. hand-in. SPb.: Epbi SPb, 2002. S. 352.
- Anzivino E., Fioriti D., Mischitelli M. et al. Herpes simplex virus infection in pregnancy and in neonate: status of art of epidemiology, diagnosis, therapy and prevention // Virol. J. 2009. Vol. 6. No. 40. P. 1–11.
- Bursrein DN Sequally transmitted treatment guidelines // Current Opin. Pediatrics. 2003 Vol. 15. P. 391–397.
- Suligoi B., Cusan M., Santopadre P. et al. HSV-2 specific seroprevalence among various populations in Rome, Italy. The Italian Herpes Management Forum // Sex Transm. Infect. 2000 Vol. 76. P. 213–214.






Add a comment