Atopic dermatitis, or eczema, is a chronic, itchy skin condition that is associated with dry skin. It usually begins in infancy or childhood and is often associated with other atopic conditions such as asthma and allergic rhinoconjunctivitis (hay fever).
Atopic dermatitis affects up to 20–30% of children and 2–10% of adults. People with a personal or family history of atopy, a tendency to develop allergic conditions, are more prone to atopic dermatitis. At estet-portal.com read how the barrier function of the skin changes with atopic dermatitis.
- What causes atopic dermatitis
- How the skin barrier normally functions
- What factors support the protective function of the skin
- How the immune system and the microbiome affect barrier functionskin
What causes atopic dermatitis
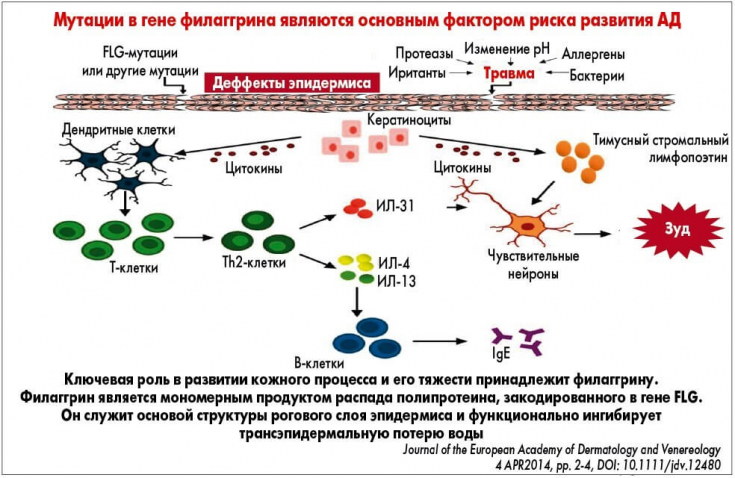
The causes of atopic dermatitis are not fully understood. The main cause of atopic dermatitis is believed to be impaired skin barrier function and a predisposition to allergic inflammation. Environmental triggers cause an allergic reaction that aggravates the symptoms of atopic dermatitis.
Immunological disorders occur in T lymphocytes, in particular in T helper type 2 (Th2) cells in the acute phase and in Th1, Th17 and Th22 cells in chronic lesions. Th2 cells produce interleukins: IL-4 and IL-13, which enhance the production of immunoglobulin E.
One theory for the pathogenesis of atopic dermatitis is the "inside-out theory", in which the immune system is believed to be the main problem and the skin barrier becomes dysfunctional secondary to IgE sensitization.
Read the most interesting articles in Telegram!
Another theory is the "external theory" where the initial defect is thought to be in the skin, resulting inan increase in allergen exposure and subsequent IgE sensitization.
How the skin barrier normally functions
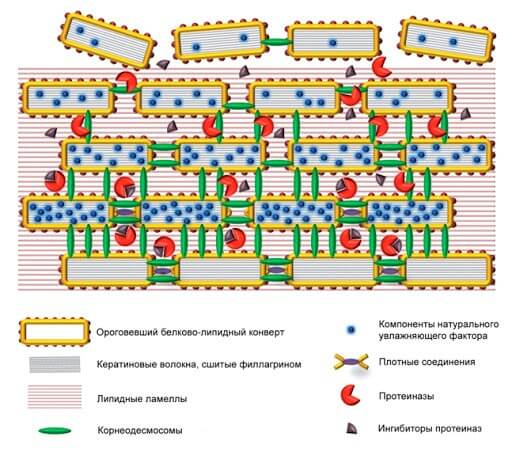
The skin barrier provides protection against external threats such as pathogens, chemicals, irritants and allergens that can trigger an immune response. The skin barrier also protects the body from epidermal water loss, and skin barrier function can be measured by the rate of transepidermal water loss.
Increased transepidermal water loss corresponds to increased skin permeability.
Skin barrier function can be measured by:
- surface pH;
- tracing connections permeability;
- cohesion of the stratum corneum;
- hydration of the stratum corneum.
Effective treatment of atopic dermatitis: modern methods
Altered homeostasis of the stratum corneum in patients with atopic dermatitis results in increased water lossand increased penetration of allergens.
What factors support the protective function of the skin
In atopic dermatitis the structure and composition of both corneocytes and the extracellular lipid matrix of the stratum corneum can be affected in the following ways:
- loss or decrease in function of filaggrin protein (FLG);
- increased activity of serine proteases;
- lipid mantle disorder.
Filaggrin is important for the structural integrity of the stratum corneum. It aggregates keratin filaments within corneocytes and then helps form the cornified cell sheath surrounding the corneocytes. FLG degradation products also contribute to the moisture retention capacity and acidic pH of the stratum corneum.
Maintaining an acidic pH is important in regulating enzyme activity that leads to desquamation, lipid synthesis, and inflammation.
Loss-of-function mutation in the FLG gene is the strongest genetic risk factor for atopic dermatitis. FLG mutations are associated with earlier onset of atopic dermatitis, greater disease severity, and persistence of the disease.
Lifestyles to choose for atopic dermatitis
The activity of serine proteases, such as kallikreins (KLK) 5 and 7, is regulated by the pH of the stratum corneum. KLK5 and KLK7 cleave extracellular corneodesmosomal proteins that bind corneocytes together. Their increased activity leads to a decrease in adhesion and desquamation of corneocytes.
The normal pH of the skin is acidic and limits the activity of these proteases, which are more active in an alkaline environment. With atopic dermatitis, the pH of the skin increases, and then the activity of serine proteases.
The lipid matrix of the stratum corneum consists of three types of lipids – cholesterol, free fatty acids and ceramides. They form a highly ordered structure of densely packed lipid layers. This extracellular lipid matrix is the main pathway for substances to pass through the skin barrier.
New options for the treatment of atopic dermatitis in children and adults
In atopic dermatitis, there is a decrease in total lipids, a significant deficiency of certain types of lipids, and changes in the composition of lipids. In combination, this leads to a violation of the barrierfunction of the skin and an increase in the permeability of the stratum corneum.
How the immune system and the microbiome affect the barrier function of the skin
A defect in the skin barrier can allow the transfer of allergens or haptens (molecules that cause an allergic reaction only when bound to a protein) into the skin, resulting in the release of pro-inflammatory cytokines that cause skin inflammation.
At the same time, the Th2 cytokines IL-4 and IL-13 and the Th2 cytokine IL-22 suppress the expression of filaggrin, causing further damage to the skin barrier.
Skin microbiome – these are pathogenic and commensal bacteria, fungi and viruses that live on our skin and help maintain epidermal homeostasis. More than 90% of patients with atopic dermatitis have skin colonized with Staphylococcus aureus.
Difficulties and errors in diagnosing atopic dermatitis in children
When the stratum corneum is structurally competent, with acidic pH and a well organized lipid matrix, it prevents colonization by pathogens such as S. aureus.

S. aureus surface proteins reduce the production of free fatty acids in the epidermis, resulting in increased skin permeability.
In patients with atopic dermatitis, superantigenic S. aureus exotoxins stimulate IgE production and cause itching. Subsequent irritations create additional skin barrier defects.
More useful and interesting information on our channel on YouTube:







Add a comment