Plastic surgeons note that in recent years the number of patients admitted with deep and extremely severe burns has increased, which requires high qualification and a special surgical approach to save severely burned patients. Active surgical tactics, including a clear algorithm for the doctor's actions when a severe patient with burns is admitted, can significantly expand the survival of such patients.
The vast experience accumulated in the world of local treatment of patients with burns allows us to formulate some undeniable postulates at the present time.
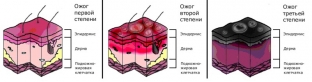
• Local treatment of superficial burns of I-II degree, even extensive ones, does not present serious difficulties. When treated by any means, they heal within 7-12 days.
• IIIA degree subdermal burns require a longer conservative therapy, which does not exclude the possibility of using surgical treatment in a limited number of patients. Such burns heal within 3 to 6 weeks.
• Deep IIIB-IV degree burns require surgical treatment.
• Local conservative treatment of deep burns is only auxiliary, it aims to prepare the burn wound for free skin grafting as soon as possible - the final stage in restoring the lost skin.
First Aid for Burns
In the prehospital setting, for localized burns, a dry aseptic dressing is the best primary dressing; for extensive burns, standard contour dressings or sterile drapes are used for this purpose.
The initial dressing should be free of fats and oils due to subsequent difficulties in wound dressing, as well as dyes, because. they can make it difficult to recognize the depth of the lesion. The most effective measure at the prehospital stage is cryotreatment of burn surfaces. This is achieved by pouring cold water on the affected area for 10-15 minutes or using ice, snow in a clean plastic bag or a ready-made cryo bag for this purpose.
Cryotreatment stops the effect of the thermal agent on the tissue of the victim and contributes to the favorable course of burns in the future.
Upon admission to the burn center, the victims undergo primary treatment of burn wounds, the nature and volume of which depends on the area and depth of the burn lesion. In the presence of limited superficial burns (no more than 20% of the body surface) without signs of burn shock, a thorough toilet of burn wounds is usually performed, which consists in removing the desquamated epidermis, foreign bodies, blisters, in abundant washing with antiseptic solutions and applying an ointment dressing.
If extensive skin burns accompanied by shock are present, no initial treatment is performed on admission. The patient is wrapped in a sterile sheet, and a delayed primary toilet is performed after stabilization of the general condition. Deep burns are treated in the same way as superficial ones, with the only difference being that a bandage with antiseptic solutions is applied.
It is not uncommon for an urgent surgical intervention to be required upon admission. A similar situation occurs in the presence of circular burns of the neck, limbs or chest. In these cases, with a scalpel without additional anesthesia, a longitudinal dissection of the scab (necrotomy) is made to viable bleeding tissues. Such a simple manipulation leads to an improvement in the blood supply to the affected areas, prevents the deepening of the burn lesion, and in case of chest burns, it significantly improves respiratory excursions.
How to Treat Deep Burns
Local treatment of deep burns has its own specific tasks in different phases of the course of the wound process. Shortly after receiving a burn in the period of acute inflammation and suppuration, treatment is aimed at combating wound infection and should contribute to accelerated rejection of necrotic tissues. For this, frequent (up to daily) dressings are carried out with solutions of iodine-containing drugs (iodopyrone, iodovidone, povidone-iodine, etc.), chlorhexidine, dioxidine, furacilin, poviargol, lavasept, plevasept, etc.
The modern antiseptic miramistin, which is used in 0.01% concentration, has proven itself well to fight infection (S.V. Smirnov, L.P. Loginov, 2000). In the first phase of the wound process, in the presence of wet scabs or during the period of their active mechanical removal, carbon dressings are used.
These materials have a good sorption capacity, which leads to a decrease in purulent discharge, drying of scabs and, as a result, a significant decrease in body intoxication. At the end of this phase of the wound process, water-soluble ointments (Levomekol, Dioksikol, Silvatsin, etc.) are also used to fight infection.
In order to reject dead tissues, proteolytic enzymes of animal origin (trypsin, chemotrypsin, pancreatin), bacterial enzymes (streptokinase, collagenase, terrilitin, etc.), plant enzymes (papain, etc.) are used. The fact that enzymes do not act on a dense burn eschar should be taken into account. Therefore, the use of enzymes is most indicated in the process of mechanical removal of necrosis or in the presence of wet scabs.
Keratolytic agents (lactic, salicylic, carbolic acids, urea) are of limited use in our practice, since they increase the local inflammatory process in the wound, causing increased intoxication. These funds are used by us only for limited burns in victims who are not subject to surgical treatment for one reason or another (refusal to operate, severe concomitant pathology).
With conservative treatment of deep burns, spontaneous rejection of non-viable tissues can be expected only 4-6 weeks after the injury. Such long periods of preparation of burn wounds for free skin grafting - the final stage of surgical treatment of burned patients - are unacceptable, since during this time the condition of patients may worsen due to the addition of complications, and the operation becomes problematic for many of them.
Therefore, we, like combustiologists around the world, strive to close wounds with autografts as soon as possible. This is achieved by surgical methods of treatment: necrotomy, necrectomy and free skin grafting. The ideal method of surgical treatment of deep burns is the radical excision of non-viable tissues with simultaneous skin plasty of the formed defect in the first 2-3 days after the burns.
However, the difficulty of diagnosing the depth of the lesion, the traumatic nature of the operation itself, the lack of confidence in the complete removal of dead tissues lead to the fact that it can be performed only in a limited number of burned patients with a deep burn area of no more than 10% of the body surface.
For more extensive lesions, surgical removal of burn eschar is usually performed in several stages. Usually, on the 3-5th day after the relief of burn shock and stabilization of the main indicators of homeostasis, under general anesthesia, the first stage of necrectomy is performed, in which part of the scabs is removed using a rotary dermatome or Gumby knife. The area of scabs removed at once is determined by the age, condition of the patient and the total area of the deep burn.
Usually, for extensive burns, 1/2-1/4 of the scabs are removed in the first stage, and the remaining scabs are removed in the second and third stages. The operation is performed with mandatory compensation of intraoperative blood loss. Over the past 8-10 years, there has been a sharp increase in victims with severe and extremely severe burn injuries. In this regard, mutilation operations (amputations of limbs) have become commonplace in burn hospitals.
To remove the remnants of non-viable tissues, frequent (up to daily) dressings with antiseptic solutions, enzymes, and antibiotics are used. In the future, with the beginning growth of granulation tissue, they switch to ointment dressings (2% furatsilin ointment, levomekol, dioxicol, etc.). Lavendula ointment, containing the antiseptic miramistin and the enzyme of bacterial origin ultralysin, has proven itself well. Miramistin well suppresses gram-negative and gram-positive microflora, and ultralysin promotes proteolysis and removal of the remaining dead tissues.
In the same period, various ointments on a knitted mesh basis are used. Among them, single-layer ointment dressings with 5% dioxidine ointment deserve attention. Usually, after 2-3 dressings, we could note a decrease in purulent discharge, activation of the growth of granulation tissue, and a decrease in microbial contamination of burn wounds. An important advantage of this dressing is that it is easily and painlessly removed from the surface of the wound at the next dressing.

In the same phase of the wound process (regeneration), drugs that stimulate the growth of granulations are used: wipes with hyaluronic acid, balsamic dressings, etc. Pigskin xenotransplantation has not lost its value for temporary covering of extensive burn surfaces in order to protect them from nosocomial infection and reduce the loss of proteins, electrolytes and fluids.
Skin grafting for burns
An indicator of the readiness of the wound to close it with autografts is the presence of a bright red granulation cover with a mild purulent discharge with a pronounced border of marginal epithelization, the absence of remnants of non-viable tissues.
A prerequisite for free skin grafting is the absence of hypoproteinemia (total protein not less than 60 g/l), hypoalbuminemia (protein coefficient not less than 1), anemia (hemoglobin not less than 90 g/l). A temporary contraindication to surgery is the presence of b-hemolytic streptococcus in the wound. We resort to the removal of granulations before autodermoplasty extremely rarely, since it is almost always possible to achieve a good condition of the latter and there is hope for a good engraftment.
Burn wounds on an area up to 15-20% of the body surface are usually closed in one stage, more extensive burn wounds need 2-3-, and sometimes 4-5-stage operations. Skin flaps are cut with manual or electric dermatomes under general anesthesia.
The problem of donor resource shortage is solved with the help of mesh autodermal grafts with a stretch ratio from 1:2 to 1:6. Repeated cutting of skin flaps from a healed donor site also solves the problem of a shortage of donor resources. Rapid epithelialization of donor wounds is facilitated by the application of single-layer ointment dressings with 5% dioxidine ointment after surgery: with a cut graft thickness of 0.3 mm, donor wounds were epithelialized in 10-12 days. All burn wounds are closed with autografts within 2-2.5 months from the moment of the burn injury.
In the postoperative period, local treatment also did not lose its significance. We are talking about patients who have a partial melting of skin flaps and the formation between them of many granulating wounds. In this situation, various spongy coatings (colaspon, digispon, biotrauma, geshispon, etc.) are useful, which can not only really stimulate reparative processes, but also have an anti-inflammatory effect. Unfortunately, at present, many of them are not produced by the domestic industry due to the difficult economic situation in the country. To combat excessive granulations, we use hydrocortisone ointments.
The surgical treatment of extensive deep burns described above fits into the concept of "active surgical tactics", formulated 40 years ago by N.I. Atyasov. In the process of surgical treatment of the burnt, physical methods of influencing the wound process (UHF, UVR, laser therapy, Klinitron beds, ceilings with infrared radiation, etc.) have not lost their significance. Local treatment of extensive deep burns is carried out against the background of intensive infusion-transfusion therapy, which allows maintaining homeostasis indicators within normal values.
Thus, active surgical tactics made it possible to improve the results of treatment of severely burned patients, expand the survival rate for extremely severe burns, save the lives of some patients with deep burns on an area of 50 - 60% or more of the body surface.
According to rmj.ru







Add a comment