Desquamative inflammatory vaginitis — is a newly recognized clinical syndrome characterized by persistent purulent vaginal discharge and vaginal erythema, often with submucosal cervicovaginal petechiae.
Inflammation is the main feature of this disorder, which is also called idiopathic inflammatory vaginitis. However, the term "desquamative inflammatory vaginitis" takes precedence and was first introduced in 1965 by Gray and Barnes. The term "aerobic vaginitis" was introduced in 2002 after the association of the disease with an abnormal vaginal microbiome.
In the article estet-portal.com you can get acquainted in detail with the management of desquamative inflammatory vaginitis according to modern recommendations.
What causes desquamative inflammatory vaginitis
The exact cause of desquamative inflammatory vaginitis is unknown, but it appears to be a dysbiosis of the vaginal microbiome associated with inflammation.
In desquamative inflammatory vaginitis, the vagina is colonized by facultative bacteria rather than the obligate anaerobic bacteria that colonize the vagina in bacterial vaginosis.
The microflora in desquamative inflammatory vaginitis usually consists of Escherichia coli, Staphylococcus aureus, group B streptococcus, or Enterococcus faecalis. Desquamative inflammatory vaginitis may also result from a systemic inflammatory syndrome that causes inflammation of the vagina, resulting in abnormal vaginal flora.
Watch the most interesting videos on our
Clinical manifestations of desquamative inflammatory vaginitis include purulent vaginal discharge and a severe inflammatory reaction. Vaginal discharge is homogeneous and yellowish, without a fishy odor. In severe cases, vulvar irritation and erythema of the vaginal mucosa with ecchymotic lesions or erosions are present. Symptoms may last for a long time, suggesting a chronic or relapsing course.
The prevalence of desquamative inflammatory vaginitis in women is between 2 and 20%.
Diagnostic features of a patient requiring treatment for vaginitis
Microscopic examination of vaginal preparations of vaginal secretion shows an increase in inflammatory cells and parabasal epithelial cells, and the vaginal flora is usually abnormal with an elevated pH.
Diagnosis is based on the presence of an elevated white blood cell count and parabasal epithelial cells. Microscopic examination of wet slides is the preferred method for diagnosing desquamative inflammatory vaginitis, as Gram staining of the vaginal flora does not distinguish between bacterial vaginosis and desquamative inflammatory vaginitis.
This disorder has been associated with an increased risk of preterm birth, premature rupture of membranes, chorioamnionitis, and miscarriage.
Recommendations for the treatment of desquamative inflammatory vaginitis
Clindamycin is active against a wide range of facultative bacteria associated with desquamative inflammatory vaginitis and also has anti-inflammatory effects. In clinical practice, topical clindamycin, often used as long-term maintenance therapy, is an effective treatment for severe forms of desquamative inflammatory vaginitis. Maintenance therapy once a week is usually used to reduce the risk of relapses or exacerbations.
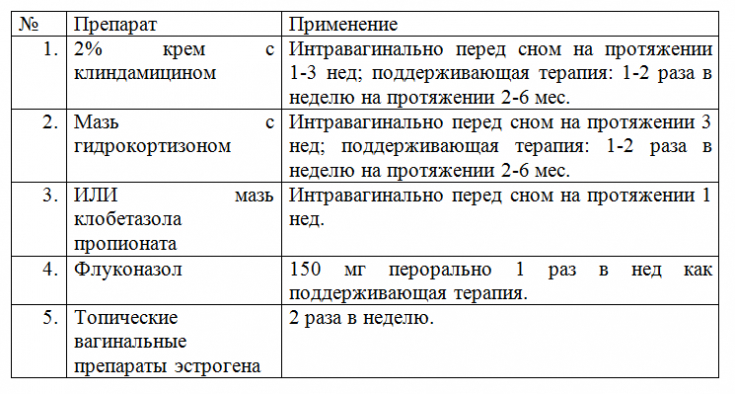
For women with desquamative inflammatory vaginitis with a prominent parabasal cell component, intravaginal estrogens (maintenance therapy) may be effective. Official guidelines for the treatment of desquamative inflammatory vaginitis have not been developed and implemented.
Metronidazole is not effective in desquamative inflammatory vaginitis.
Thank you for staying with estet-portal.com. Read other interesting articles in the "Gynecology" section. You may be interested in
Bacterial vaginosis: a very unpleasant disease of young women







Add a comment