Diabetic ketoacidosis − acute, life-threatening complication of diabetes mellitus, characterized by the development of hyperglycemia, ketoacidosis and ketonuria. Diabetic ketoacidosis develops more often in patients with type 1 diabetes mellitus, but it is also often observed in type 2 diabetes.
This publication on estet-portal.com highlights the key points of the pathogenesis of diabetic ketoacidosis, as well as the features of laboratory diagnosis of this pathological condition.
Etiology of diabetic ketoacidosis in diabetes mellitus
The most common factors that lead to the development of diabetic ketoacidosis in patients with diabetes mellitus are the presence of concomitant infection (40%), missed insulin doses (25%), recently diagnosed diabetes mellitus and lack of adequate treatment (15%), other reasons (20%).
Follow us on Instagram!
In patients with type 1 diabetes, ketoacidosis is most often the result of:
1) Acute insulin deficiency (occurs in 25% of patients with type 1 diabetes mellitus);
2) Poor compliance due to a low level of education or against the background of psychological protest to treatment (in adolescents);
3) Missing another dose;
4) Associated bacterial infection, including pneumonia caused by Klebsiella pneumoniae (the leading cause of infections accompanied by diabetic ketoacidosis);
5) Emotional stress;
6) Insulin pump malfunctions.
Osteoarthritis as a complication of diabetes
The development of diabetic ketoacidosis in patients with type 2 diabetes mellitus is most often associated with such conditions: intercurrent diseases (for example, myocardial infarction or pneumonia), the use of drugs (in particular, corticosteroids, clozapine, pentamidine).
Diabetic ketoacidosis often occurs in pregnant women with diabetes mellitus: the physiological changes characteristic of pregnancy are a favorable background for the development of ketoacidosis.
Pathophysiology of diabetic ketoacidosis in diabetes mellitus
Diabetic ketoacidosis occurs against the background of an absolute or relative deficiency of insulin and as a result − inability of cells to absorb glucose. Energy starvation of cells is a signal for the activation of hormones: glucagon, cortisol, growth hormone, adrenaline. Hormones, in turn, activate gluconeogenesis in the liver, glycogenolysis and lipolysis. All these processes lead to an even greater increase in the level of glucose in the blood, as well as the level of free fatty acids (due to lipolysis).
Free fatty acids − alternative source of energy: their increased metabolism in the liver is accompanied by the production of an excess of intermediate and final metabolites, in particular acetone, beta-hydroxybutyrate and acetoacetate.
Ketonemia and ketonuria lead to the development of metabolic acidosis with a significant decrease in serum pH and bicarbonate levels. Respiratory compensation of acidosis is clinically manifested by Kussmaul breathing.
Ketones, in particular beta-hydroxybutyrate, induce nausea and vomiting, leading to loss of fluid and electrolytes in the face of an already existing deficiency.
Glycosuria, characteristic of diabetic ketoacidosis, leads to increased diuresis, dehydration and hyperosmolarity of blood plasma. Due to decompensated dehydration, prerenal renal failure develops.
Therapeutic Strategies for the Development of Insulin Analogs
Hyperglycemia, osmotic diuresis, serum hyperosmolarity and metabolic acidosis induce severe electrolyte disturbances. A characteristic electrolyte disorder is hypokalemia. The cause of hypokalemia is an increased transition of potassium from the intracellular to the extracellular space in exchange for hydrogen ions, which accumulate in excess during acidosis.

A significant part of the potassium is lost due to osmotic diuresis. Serum hyperosmolarity, dehydration and acidosis lead to an increase in osmolarity in brain cells, which is clinically manifested by a change in the level of consciousness.
Diabetic ketoacidosis: clinical picture and diagnosis
Early clinical symptoms of diabetic ketoacidosis are increased polydipsia and polyuria. Other signs of diabetic ketoacidosis include the following: weakness, fatigue, nausea and vomiting, which may be associated with diffuse abdominal pain, loss of appetite and anorexia, decreased sweating, dry skin, altered level of consciousness (partial disorientation). Coma is rare and occurs with severe dehydration/acid-base disturbance.
Progressive methods of diabetes treatment
An objective examination of a patient with ketoacidosis may reveal: dry skin and mucous membranes, reduced skin turgor, hyporeflexia, a characteristic acetone odor, tachycardia, tachypnea, hypotension, hypothermia.
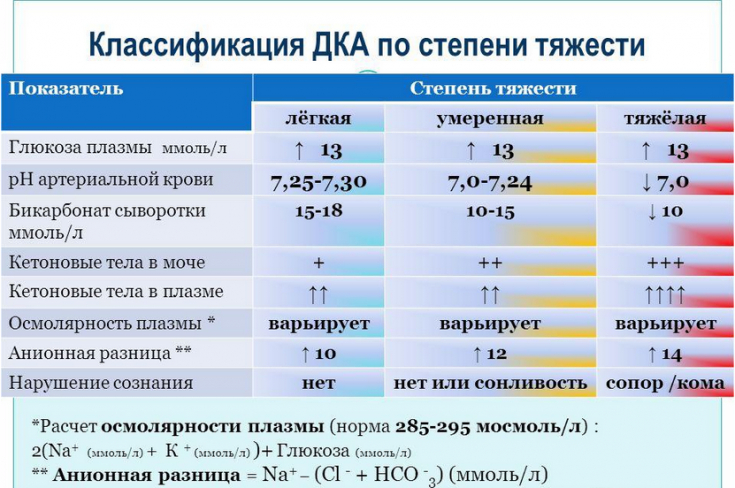
Patients with suspected ketoacidosis should have the following levels checked: serum glucose, serum electrolytes (potassium, sodium, chloride, magnesium, calcium, phosphorus), bicarbonates, lipase and amylase, capillary blood/serum ketone bodies blood, urea and creatinine.
In addition, patients with diabetic ketoacidosis need a complete blood and urine test, as well as an ECG.
Instrumental imaging may be useful in the following situations:
1. Chest x-ray − to exclude the diagnosis of pneumonia.
2. Computed tomography (CT) or magnetic resonance imaging (MRI) of the brain − for early detection of edema.
Neuropathic ulcer as a complication of diabetes
Hypertonic saline or mannitol should not be delayed pending brain CT or MRI results if cerebral edema is suspected.
Ketoacidosis is a very dangerous condition that requires careful timely diagnosis to prevent possible complications such as coma or cerebral edema.
The hormone melatonin may increase the risk of diabetes







Add a comment