Despite the different origin of scleroderma diseases, almost all of them at the beginning of their development can have a similar clinical picture, which makes it difficult to diagnose them early, requires the doctor to have knowledge of clinical manifestations, the ability to carefully collect anamnesis, and examine patients in detail using modern diagnostic methods.
Considering that in diffuse diseases of the connective tissue, skin lesions are among the permanent symptoms and are extremely diverse, and there are very few specific nosological signs, in terms of diagnostics, the scleroderma-like disease "Buschke's scleroderma" (edematous scleroderma, progressive benign subcutaneous induration, adult scleroderma) is a rare skin disease of unclear etiology, characterized by dense diffuse swelling of the dermis and subcutaneous tissue.
The literature indicates two peaks of incidence: at the age of one to twenty years and from forty-one to fifty; women are affected twice as often as men. The onset of the disease is almost always associated with some kind of infection of the upper respiratory tract (angina, tonsillitis, pharyngitis, scarlet fever, measles, whooping cough, influenza, pneumonia). In some patients, the disease occurs after a severe injury. A number of authors believe that an infectious-toxic or infectious-allergic process plays an important role in the development of Bushke's scleroderma.
We present a case of Buschke's scleroderma diagnosis.
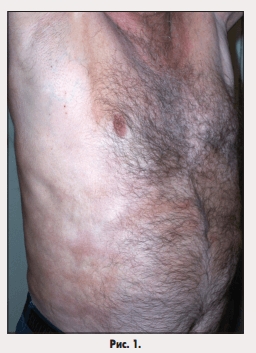
Patient M., male, 69 years old, retired. He was admitted to the rheumatology department of the Luhansk City Clinical Multidisciplinary Hospital No. 1 in March 2011 with skin thickening and a feeling of tightness in the upper back, anterior abdominal wall (Fig. 1), stiffness in the neck. He fell ill in October 2010, when hyperpigmentation and thickening of a skin area in the area of the right shoulder blade with a diameter of about 15 cm was first noted. He did not seek medical help, he applied paraffin applications. Gradually (within a few months), the seal spread to the upper back, the lateral surfaces of the abdomen. In March 2011, when contacting a dermatologist, systemic scleroderma was suspected, in connection with which the patient was referred to a rheumatologist. It was not possible to clarify the causes of this disease.
History: pulmonary tuberculosis since 2005, staghorn stone in the left kidney. Allergological and hereditary anamnesis is not burdened. For 20 years he worked as a drifter in a mine.
Objective examination data. General condition is satisfactory. Consciousness is clear.
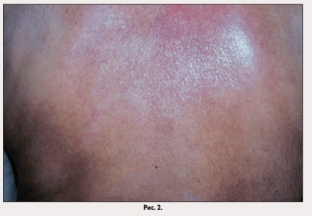
Body temperature 36.7°C. The skin in the area of the upper back and the back of the neck is significantly thickened, not taken into a fold, devoid of its normal pattern. The defeat is symmetrical. The skin is stretched, hyperemic (Fig. 2). Areas of skin compaction in the area of the anterior abdominal wall are pale with areas of hyperemia. Facial skin is not affected, facial expressions are preserved, mouth opening is free. There are no areas of atrophy, skin sensitivity is not disturbed. There is no hairline in areas with altered skin.
Analysis of the results of additional research methods confirmed the absence of a systemic lesion and made it possible to make a differential diagnosis of the present disease with eosinophilic fasciitis and Werner's syndrome.
Diagnosis. Taking into account the characteristic symmetrical changes in the skin in the form of its significant compaction, tension and hyperemia in the upper back, posterior surface of the neck and anterior abdominal wall, the absence of a normal skin pattern and the possibility of its fold formation with normal facial skin, preserved facial expressions, as well as the absence of systemic signs process, taking into account the data of the histological examination of the skin flap (thickening of the dermis, moderate hyalinosis of collagen fibers, hair follicles, sweat and sebaceous glands are atrophied, in the subcutaneous tissue - the growth of hyalinized collagen fibers, minor inflammatory infiltrates - around the vessels, the walls of the vessels of the dermis are sclerosed) and based on the results of the differential diagnosis with other scleroderma-like diseases,
Treatment. The basis of therapy for Buschke's scleroderma is glucocorticoids, antifibrotic drugs, and if necessary, symptomatic treatment is used. After the diagnosis was made, the patient was prescribed methylprednisolone at a daily dose of 16 mg for a month, followed by a dose reduction of 2 mg every 10 days.A month later, positive dynamics was noted, which manifested itself in a decrease in skin density in the neck, back, lateral surface of the abdomen, and improved mobility in the neck and back. The patient is under dynamic observation and continues treatment with methylprednisolone at a dose of 8 mg per day.
Discussion. The prognosis for life with Bushke's scleroderma is favorable. Researchers of this problem note the possible spontaneous resolution of the disease within a few years. Patients with Buschke's scleroderma are subject to observation by a rheumatologist with dynamic control of clinical, laboratory and instrumental data.
In presenting this clinical case, we hope to draw the attention of doctors of various specialties to the diversity of scleroderma-like diseases and the features of skin manifestations in the absence of systemic lesions. The alertness of specialists in relation to this group of diseases will contribute to the timely referral of these patients to a rheumatologist, early diagnosis and high-quality treatment with basic drugs.
According to health-ua.com








Add a comment