Melasma – violation of pigmentation in areas of the skin exposed to sunlight. On the face, it is customary to distinguish three types of melasma: central facial, malar and mandibular.
The causes of dark spots at the molecular level remain largely unexplored, however, in addition to ultraviolet radiation, hormonal effects and genetic predisposition are among the provoking factors.
In this article, Dr. Clare Amrani provides an overview of the available treatments for melasma based on the evidence available to date.
- Relevance of classification of melasma according to histological features
- Overview of all existing strategies for melasma treatment
Relevance of classification of melasma according to histological features
Until recently, it was customary to distinguish three histological types of melasma:
• epidermal;
• dermal;
• mixed.
This simple classification made it possible to clearly identify the type of melasma and select the appropriate treatment plan with predictable results. Dermal melasma is the most difficult to treat and is characterized by frequent relapses.
However, recent studies using electron microscopy, immunocytochemistry, and confocal microscopy in vivo have shown that in fact any melasma is mixed, since melanin and melanophages are not homogeneously distributed in the skin.
Therefore, melasma cannot be exclusively epidermal; pigmentation disorder – complex pathology involving epidermal cells, keratinocytes, melanocytes, fibroblasts, as well as vascular endotheliocytes.
The vascular network in areas of the skin affected by melasma is denser. This concept will be explored in more detail in future research.
Recent studies have shown that in fact any melasma is mixed.
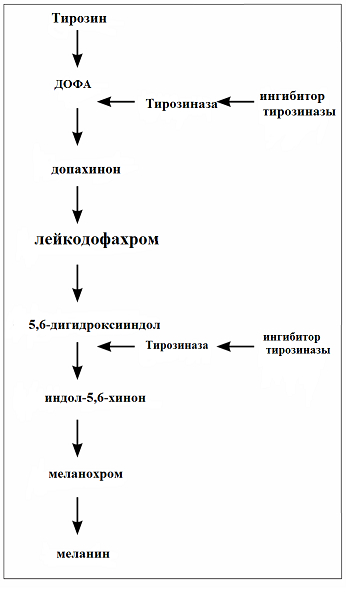
Fig. 1: melanin production: the role of tyrosinase inhibitors
Overview of all current melasma treatment strategies
The treatment of melasma is based on four main principles: skin photoprotection, application of topical preparations, oral preparations and the use of invasive techniques.
Correction of hyperpigmentation: the choice of effective treatments for melasma
1. Photoprotection
Ultraviolet exposure – one of the main etiological factors of melasma. Therefore, protection from sunlight all year round – a must-have addition to any therapy. It has been shown that the risk of recurrence of melasma is significantly increased in the absence of adequate photoprotection of the skin.
2. Topical remedies
Hydroquinone
Drug treatment is aimed at inhibiting tyrosinase – an enzyme that plays a key role in the production of melanin (Fig. 1). Most often, hydroquinone is used in topical therapy for melasma, which performs this function, and can also contribute to the degradation of melanocytes and negatively affect the synthesis of DNA and RNA in melanocytes. The effectiveness of hydroquinone is directly proportional to its concentration (optimal – 4%).
Retinoids
Retinoids reduce melanin production in two ways:
- inhibit tyrosinase transcription;
- when used in combination with hydroquinone, they reduce the degree of oxidation of hydroquinone, enhancing its epidermal penetration.
Corticosteroids
Corticosteroids reduce pigmentation by affecting melanin production and also have anti-inflammatory properties. Acne and telangiectasia – long-term side effects that may occur with the use of corticosteroids. Most often, these drugs are prescribed as part of a comprehensive treatment plan.
Azelaic acid
This substance inhibits tyrosinase and also destroys abnormal melanocytes and reduces their proliferation.
Kojic acid
Kojic acid has a dual effect: it inhibits tyrosinase activity and is a powerful antioxidant. As a monotherapy, this acid is less effective than hydroquinone, but dual therapy has been shown to be effective in the treatment of melasma.
Combination use of topical preparations
The purpose of combination therapy – increase the effectiveness of one of the active substances, as well as minimize the side effects of the treatment.
Thus, retinoids reduce the oxidation state of hydroquinone, improving its penetration into tissues and reducing the concentration of hydroquinone required to obtain a result.
Steroids significantly reduce irritation caused by other substances.
Composed in 1975, the Kligman formula provides for the use of 5% hydroquinone, retinoids at a concentration of 0.1% and 0.1% dexamethasone. Changes to the formula are made taking into account the individual characteristics of the patient's skin.
Due to their mutually reinforcing effect, combination therapies are more effective and provide faster results than monotherapies.
3. Oral preparations
Tranexamic acid is most commonly used for oral administration – synthetic substance of the amino acid lysine. It is able to inhibit the conversion of plasminogen to plasmin. Plasminogen is also found in keratinocytes and cells of the basal epidermis. UV light stimulates the keratinocyte/plasminogen system, resulting in the production of prostaglandin and leukotrienes. They, in turn, stimulate the synthesis of melanin. Inhibition of melanogenesis is achieved through the ability of TXA to bind to plasminogen.
TCA can also inhibit vascular endothelial growth factors and endothelin-1, which contribute to the expansion of the vasculature. This is important in light of the new aspect of histological classification described above.
Tranexamic acid in the treatment of melasma
4. Invasive procedures
Melasma interventional therapy includes laser therapy to eliminate pigmentation and reduce the vascular network, chemical peels, microdermabrasion and microneedling.
Typically, the above procedures are combined with other therapies such as topical preparations.
Laser therapy for melasma, particularly in dark-skinned patients, is associated with a high risk of side effects, including thermal tissue damage, inflammatory pigmentation, and scarring. To solve this problem, scientists are developing a new generation of lasers. Recent studies, for example, have demonstrated the efficacy and safety of fractional picosecond laser in the treatment of melasma.
Despite the existence of various medical and interventional therapeutic tools, there is currently no single method for treating melasma and preventing its recurrence.
New knowledge obtained in the process of studying pigmentation disorders at the molecular and histological levels allows us to conclude that melasma is multifactorial.
Accordingly, melanocytes, keratinocytes, fibroblasts, vascular endothelial cells, and the molecules recreated by these cells must be treated during the treatment of melasma.
According to The PMFA Journal







Add a comment