Bacterial vaginosis is a polymicrobial synergistic infection. In this disease, the usually predominant population of lactobacilli in the vagina decreases, while populations of Gardnerella vaginalis and other anaerobes increase.
Specialists have not come to a final opinion whether it is worth treating the asymptomatic carriage of this infection, however, it is clear that in the presence of clinical manifestations, treatment of the disease is simply necessary.
At estet-portal.com, read up-to-date protocols for the treatment of bacterial vaginosis.
General principles for the treatment of bacterial vaginosis
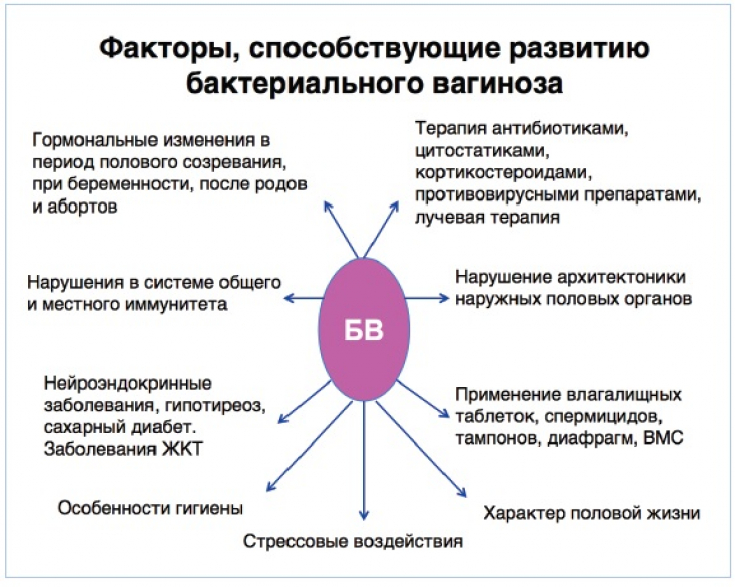
Risk factors that contribute to the development of bacterial vaginosis include:
• recent antibiotic use;
• decreased estrogen production;
• use of the intrauterine device;
• douching.
The treatment of bacterial vaginosis is not much different from the treatment of other urinary tract infections. In this disease, first of all, antibiotic therapy is prescribed.
Women who are asymptomatic carriers of Gardnerella vaginalis do not need treatment.
Treatment of bacterial vaginosis is recommended for pregnant women and before caesarean section, total abdominal hysterectomy, or IUD insertion. Uncomplicated cases of bacterial vaginosis usually respond well to standard antibiotic treatment.
Bacterial vaginosis: a highly distressing disease for young women
Clinical presentation of bacterial vaginosis and diagnosis of the disease
Typical symptoms of bacterial vaginosis include the following:
• Vaginal odor (the most common and often initial symptom of bacterial vaginosis);
• moderate gray homogeneous discharge from the vagina;
• irritation of the vulva;
• dysuria or dyspareunia;
• in most cases, no signs of inflammation.
Bacterial vaginosis is confirmed by microscopic examination of a smear by the presence of 3 out of 4 Amsel criteria:
• presence of key cells in the smear (the most specific diagnostic criterion);
• Vaginal pH above 4.5;
• characteristic gray, uniform discharge;
• appearance of a fishy smell when 10% KOH is added to the secretions.
When making a diagnosis of bacterial vaginosis, primary and secondary treatment is prescribed, the main task of which is – restore the normal flora of the vagina.
Read the latest articles in Telegram!
Bacterial vaginosis treatment protocol
Basic regimens for bacterial vaginosis are presented for primary, alternative, and adjuvant treatments, as well as specific therapies for pregnant women, patients allergic to metronidazole, and those with recurrent infection.
Treatment for primary infection:
Metronidazole per os is prescribed at a dose of 500 mg 2 times a day. within a week, or intravaginally metronidazole-gel 0.75% 1 q.d. – 5 days. Also, clindamycin cream 2% 5 g, which is administered intravaginally for a week.
Alternative treatment:
Tinidazole has a good effect in therapy, which is used according to two schemes: 2 g once a day for 2 days, or 1 g once a day for 5 days. Clindamycin 300mg q2d per week may also be given.
Pregnant:
For the treatment of pregnant women, metronidazole 500 mg per os 2 times a day is suitable. or metronidazole 250 mg orally 3 times a day
Metronidazole allergic patients:
Clindamycin intravaginal cream.
Recurrent infection:
Metronidazole Gel 0.75% 5g intravaginally twice a week for 4-6 months.
Treatment of partner for bacterial vaginosis does not reduce recurrence rate.
Additional therapy for bacterial vaginosis involves the use of probiotics to restore the vaginal flora, however, this therapy is not approved by the FDA.
Stress and bacterial vaginosis: why you shouldn't be nervous








Add a comment