With the growing popularity of contouring, there is also an increase in the number of cases of complications associated with large volumes of injected drugs, improper injection technique, etc.
One of them is filler overcorrection syndrome – excessive volumization distorting the functional anatomy and topography of the face.
This is the opinion of Dr. Song Tim >-portal.com talks about this complication, its causes, diagnosis and effective methods of correction. Possible causes of overcorrection of the face with fillers
Diagnosis of filler hypercorrection syndrome- Tactics for eliminating overcorrection with fillers
- Photos before and after hyaluronidase injection for filler hypercorrection
- mi
- Possible causes of overcorrection of the face with fillers According to the author, overcorrection may be the result of: incorrect initial assessment of a person; wrong choice of filler;
the desire to get a very pronounced lifting effect with the help of one contouring.
- The introduction of fillers into superficial fat pads or deep fat pads of areas with displaced soft tissues – the main mistakes that lead to the overcorrection syndrome.
- Read also: Bypassing Dangerous Zones: Filler Injection Points
In terms of both safety and effectiveness of the procedure,
microboluses of filler. Deep insertion of large boluses into bone structures can be hazardous even with negative retrograde needle withdrawal. Many doctors do not consider overcorrection to be a serious problem, however, structures overfilled with filler are not able to withstand gravity and aging, and with age, distortion and an unnatural appearance of the face can increase. Repeated injection of large volumes of filler can lead to excessive volumization and
pumped face effect. This may be due to a combination of the following factors:
previously injected fillers;
filler migrations;
formation of biofilms and granulomas;
delayed allergic reactions.
- In the area of the nasolacrimal sulcus, an excess of filler can distort the contours and lead to the Tyndall effect
- .
- Incorrectly selected filler, incorrect technique (for example, too superficial injection) can lead to the formation of
. They can be removed with hyaluronidase injections or, in the worst case, surgery. Large volumes of filler can also lead to the formation of foreign body granulomas.
Diagnostics of filler hypercorrection syndrome The following criteria can be used to
diagnose overcorrection syndrome:
patient had more than one contouring procedure;
patient received a bolus of more than 0.5ml filler at each site;patient has:
disruption of the normal topography of the medial infraorbital zone;
- very "heavy" lower third of the face;
- disproportionate zygomatic arch, which visually deepens the temporal zone;
- the "setting sun" phenomenon in the eye area;
- forehead too prominent;
- protruding chin;
- too voluminous lips ("duck");
- drooping of the corners of the mouth.
- Often, the diagnosis of hypercorrection is not difficult – it can be determined by the distortion of the topography of the face.
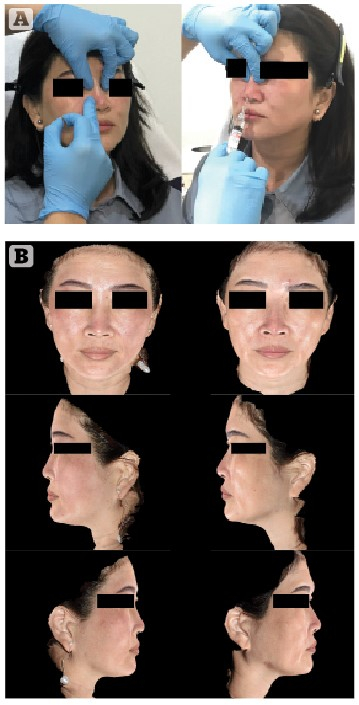
- Palpation of the problem area with the thumb and forefinger is used to
- evaluate the fluidity of the substance under the skin .
- Thus, it is possible to determine the boundaries of the
- hypercorrection focus .
The easiest way to do this is in the infraorbital zone.
The diagnosis is confirmed if, during palpation, an aggregate of soft translucent substance is detected.
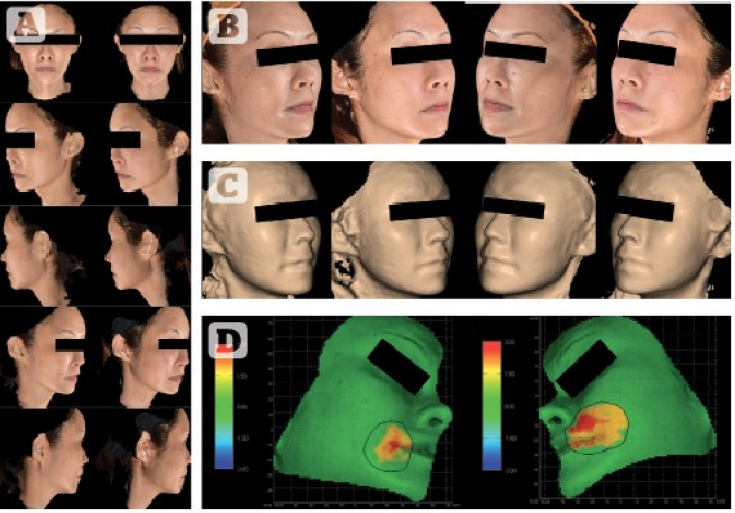
Fig. 1: diagnosis of overcorrection by palpation
diagnosis of overcorrection by palpation
Photos were analyzed using the Quantificare 3D LifeViz® system; Micro. The technology allows you to reproduce ordinary before and after photos as 3D images of the entire face to analyze volume, contours and wrinklesn.
Tactics of eliminating hypercorrection with fillers
1500 units were injected into hypercorrection areas or nodules with a 30G needle. hyaluronidase with 5 ml lidocaine. It is important that the needle breaks the integrity of the biofilm or capsule surrounding the filler during injection.
Patients were photographed at follow-up appointments 2-3 weeks and 3 months after administration of hyaluronidase
Hyalase.
It is important for the doctor to identify the layers into which the filler was injected.
However, clear drug boundaries are often difficult to define.
Therefore, injections are performed at different depths and at different angles in the hope of penetrating through biofilms or capsules and ensuring effective dissolution of the filler by hyaluronidase.
Several hyaluronidase sessions may be required for significant volume reduction.
An enzyme may be ineffective if:
fillers were in the tissues for a very long time; have been entered multiple times;
migrated a significant distancene.
- Photos before and after the injection of hyaluronidase during hypercorrection with fillers
- To eliminate hypercorrection, the filler was dissolved with hyaluronidase with lidocaine, and then re-correction was performed.
Patient 2
– hypercorrection of the middle third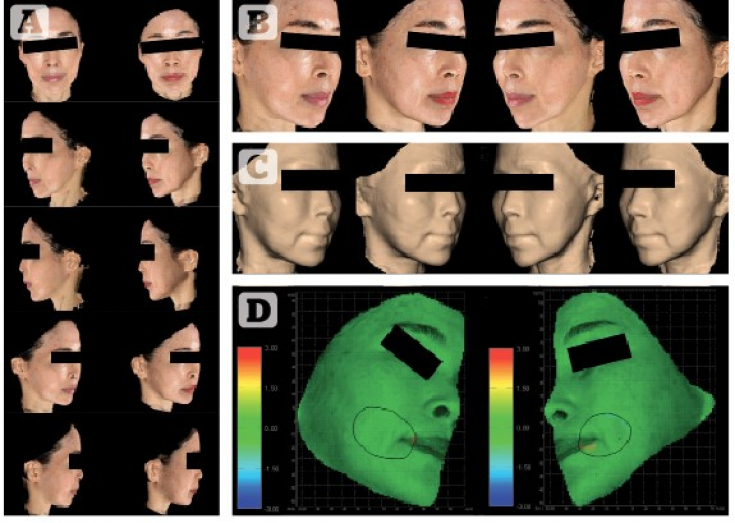
– hypercorrection of the bridge of the nose with a filler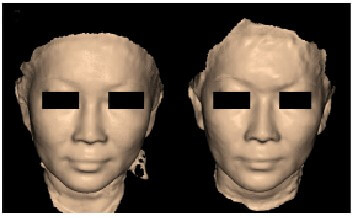
Patient 4
– hypercorrection of the middle third of the face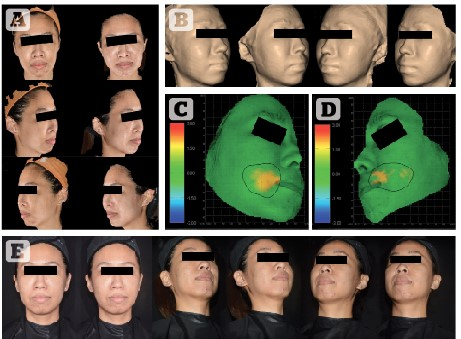
Follow us on Facebook!
In order to increase the effectiveness of anti-aging procedures and avoid overcorrection with fillers, it is necessary to assess the problem of aging and approach its solution at the level of all facial tissues.
This will most often require the use of various correction methods. Therefore, combined approaches to rejuvenation today – not a trend, but a necessity. Adapted from Prime magazine.







Add a comment