Chronic gastritis occupies a central place (more than 80% of cases) among diseases of the stomach. The discovery of Helicobacter pylori and elucidation of its role in the development of gastritis has revolutionized gastroenterology.
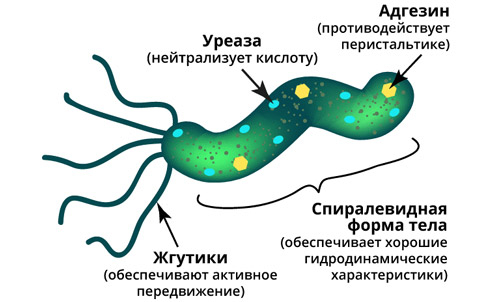
Helicobacter pylori – one of the most common chronic bacterial infections in the world.
The bacterium is the main cause of chronic atrophic gastritis and serves as the leading trigger in the development of a number of diseases of the gastrointestinal tract, including malignant ones.
Read in this article about the influence of Helicobacter pylori on the development of chronic atrophic gastritis, the main symptoms of the disease, as well as methods for diagnosing the presence of infection in the body.
Influence of Helicobacter pylori on the pathogenesis of atrophic gastritis
The main pathogenetic factors for the occurrence of chronic gastritis are the presence of Helicobacter pylori infection, as well as autoimmune mechanisms of atrophy of the gastric mucosa, which is very rare.
H.pylori provokes chronic cell damage, thereby weakening the local protective properties of the gastric mucosa.
As a result, toxins and free radicals freely penetrate tissues and damage cell nuclei. As a result of such processes, hybrid cells are formed, which can degenerate into cancer cells, resulting in intestinal metaplasia. At the initial stages of the disease, such areas of the mucosa take the form of small intestinal epithelium, and over time – colonic.
The more severe the process of metaplasia, the higher the risk of adenocarcinoma of the stomach, as a result of which Helicobacter pylori infection was included in the list of biological carcinogens. Therefore, chronic atrophic gastritis needs timely diagnosis and high-quality treatment in order not to lead to serious complications.
Follow us also in Telegram
Symptoms of chronic atrophic gastritis: main complaints
Due to a pronounced decrease in the functional activity of the stomach, in chronic atrophic gastritis, dyspepsia syndrome is the leading one, in contrast to hyperacid gastritis, where pain syndrome predominates.
Chronic atrophic gastritis syndrome includes:
1. The syndrome of gastric dyspepsia is accompanied by the appearance of heaviness and distention in the epigastric zone after eating, as well as nausea, belching of air, food, rotten eggs, an unpleasant aftertaste in the mouth and some decrease in appetite;
2. Intestinal dyspepsia syndrome is characterized by flatulence, excessive rumbling and transfusion in the abdomen, diarrhea, sometimes weight loss, hypoproteinemia and albuminemia;
3. Polyhypovitaminosis syndrome is accompanied by a deficiency of various vitamins (usually group B) and symptoms such as bleeding gums, dry skin, dermatitis and visual impairment;
4. Anemic syndrome is characterized by severe general weakness, dizziness, low levels of hemoglobin and erythrocytes, as well as an increased level of blood color index;
5. Asthenoneurotic syndrome develops more often in women: weakness, cold in the extremities, sleep disturbance, paresthesia;
6. Electrolytic imbalance syndrome occurs due to malabsorption and assimilation, which is accompanied by hypokalemia, hypocalcemia and a decrease in iron ions.
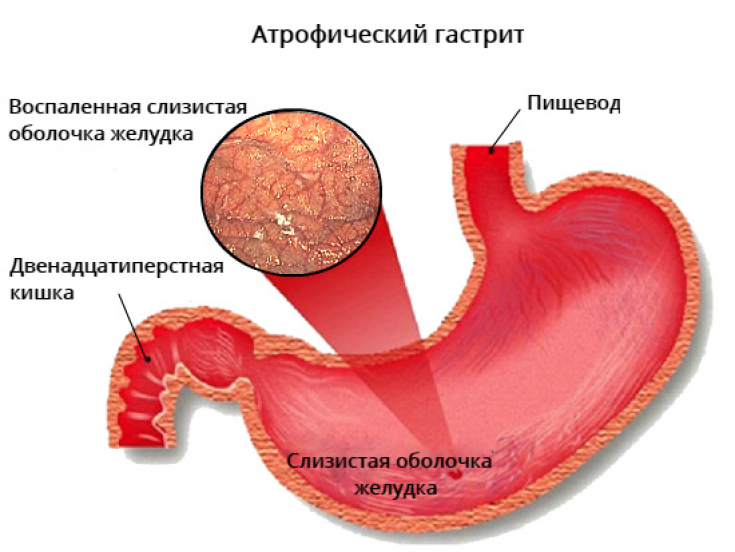
There is also pain syndrome, but not associated with spasm of smooth muscles, but with distension of the stomach due to a violation of the evacuation function of the stomach. The pains are usually dull, aching, aggravated after eating, without a clear localization.
Duodenal ulcer: treatment
Diagnosis of atrophic gastritis: popular and affordable tests
A biopsy of the stomach performed during endoscopy allows for a more accurate diagnosis. To identify Helicobacter pylori as the cause of gastritis, microscopic, urease, respiratory, serological, microbiological and histological methods are used.
Cytology – one of the most accurate methods for detecting Helicobacter pylori in the gastric mucosa.
With this method, the analysis virtually no false positive results. For research, a biopsy material is taken during fibrogastroduodenoscopy (FGDS), a smear – mucosal imprint. The result is either positive or negative.
 The fecal test is one of the most accessible methods for diagnosing an infection. Fecal analysis for Helicobacter pylori antigen is the most convenient test for the elderly, children and the seriously ill.
The fecal test is one of the most accessible methods for diagnosing an infection. Fecal analysis for Helicobacter pylori antigen is the most convenient test for the elderly, children and the seriously ill.
A breath test based on the assessment of urease activity in a biopsy specimen is also widely used. This respiratory method has its advantages:
• the result is ready in a short period of time (20-25 minutes);
• reliability of the result 90-95%;• the test does not harm the human body.This method has no contraindications, but the result will be accurate only if you properly prepare for the test.
 A blood test will also help diagnose the presence of an infection in the body based on the levels of immunoglobulins in the blood.
A blood test will also help diagnose the presence of an infection in the body based on the levels of immunoglobulins in the blood.
Helicobacter pylori: the impact of infection on the clinical course of psoriasis and eczema






