Acne vulgaris — is a chronic inflammatory disease of the pilosebaceous unit, which consists of the hair shaft, hair follicle, arrector pili muscle, and sebaceous gland. Acne primarily affects the face and, to a lesser extent, the back and chest.
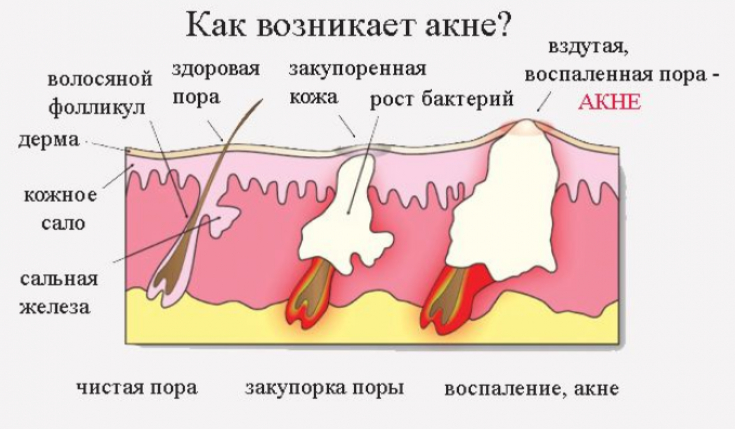
The cause of this disease is due to four main factors that interact in a complex way, leading to the appearance of acne:
• increased excretion of sebum by the sebaceous glands inside the hair follicle (seborrhea);
• follicular hyperkeratinization, which leads to the formation of a plug of sebum and keratin called microcomedone;
• bacterial hypercolonization within the pilosebaceous unit (mainly by microorganisms Propionibacterium acnes);
• innate and acquired immune responses that cause inflammation in the affected follicles.
The drug isotretinoin (13-cis-retinoic acid) is derived from vitamin A. It is available for topical and oral use. Oral isotretinoin was approved by the US Food and Drug Administration for the treatment of nodulocystic acne in 1982.
It has since revolutionized the treatment of acne and, three decades later, remains the most clinically effective anti-acne therapy.
Read more about the results of a Cochrane analysis of data from 31 randomized clinical trials of oral isotretinoinin 3836 participants (12 to 55 years old) with mild to severe acne in the estet-portal.com article . Most of the studies were conducted in Asia, Europe and North America.
Peculiarities of prescribing isotretinoin
Clinical experience with oral isotretinoin has now expanded its use to include those who are prone to scarring and those who do not improve with appropriate topical antimicrobial or retinoid-like therapies and a long course of oral antibiotics.
Follow us on Telegram!
Most physicians prescribe a daily dose of isotretinoin by mouth, which ranges from 0.5 to 1.0 mg/kg body weight; this dose allows 85% of people to get rid of acne in a maximum of 16 weeks. For the remaining patients, it takes about 5-6 months to achieve a complete response to this dose, and less than 1% of patients will require up to 12 months of continuous treatment.
Treatment regimens usually start at 0.5 mg/kg/day and may be increased to 1.0 mg/kg/day.
Since pharmacokinetic evaluations have shown that the rate of absorption can be doubled with the concomitant presence of intestinal fat, it is recommended that the capsules be taken with the main meal.
Duration of therapy is adjusted to achieve 90% acne clearance, followed by 4 weeks of maintenance therapy to consolidate treatment until drug is discontinued.
Results of a meta-analysis of the efficacy and side effects of isotretinoin
Three studies (400 participants) showed that isotretinoin was not superior to oral antibiotic plus topical treatment in terms of reducing inflammatory elements (very low-quality evidence), with only one major adverse effect found — Stevens-Johnson syndrome in the isotretinoin group.
Isotretinoin may slightly improve (15%) the severity of the condition as assessed by a dermatologist (351 participants; 2 studies), but results in side effects (67% higher risk) (351 participants; 2 studies) (e.g., dry lips/skin, cheilitis, vomiting, nausea) (low-quality evidence).
Isotretinoin is the only therapy that addresses all of the primary causative factors of acne.
One study (154 participants) reported a 79%, 80%, and 84% reduction in total inflammatory lesions after 20 weeks of 0.05, 0.1, or 0.2 mg/kg/day, respectively, for severe acne (low-quality evidence).
Isotretinoin for 24 weeks at (a) continuous low dose (0.25 to 0.4 mg/kg/day), (b) continuous regular dose (0.5 to 0.7 mg/kg/day) day) and (c) an intermittent treatment regimen (0.5 to 0.7 mg/kg/day, for one week per month) has been shown to be beneficial when using continuous treatment (low-quality evidence).
14 studies (906 participants, severe and moderate acne) reported no serious side effects when comparing different doses/treatment regimens with oral isotretinoin during treatment (12 to 32 weeks) or post-treatment follow-up (up to 48 weeks) ).
13 studies (858 participants) analyzed the incidence of less serious side effects, which included dry skin, hair loss, and itching, but heterogeneity in outcome estimates ruled out a true answer (low- or very-low-quality evidence when assessed).
After starting treatment, oral isotretinoin activates tumor suppressor genes in the skin; in the sebaceous glands, apoptosis is induced and the cell cycle stops.
Is Isotretinoin Justified
There is no conclusive evidence that isotretinoin improves the condition of an acne patient compared to a standard oral antibiotic and topical treatment as measured by overall reduction in inflammatory lesions. Only one serious side effect was reported in the isotretinoin group, however, isotretinoin may cause more minor side effects.
Isotretinoin does not cause antibiotic resistance in bacteria.
Thank you for staying with estet-portal.com. Read other interesting articles in the "Dermatology" section. You may be interested in What medications can cause drug-induced acne







Add a comment