Antiphospholipid syndrome is a whole range of disorders that are provoked by the development of an autoimmune type reaction to the phospholipid structures of cell membranes. This syndrome is found in 4% of practically healthy people. More often, antiphospholipid syndrome is diagnosed in women.
The pathogenetic causes of the development of antiphospholipid syndrome have not been established. However, factors have been identified that contribute to an increase in the level of antibodies to phospholipids. What causes APS? How can the syndrome affect pregnancy? Find out the clinical manifestations of the syndrome and its treatment methods in our article.
Factors and causes of the development of antiphospholipid syndrome
Antibody titers increase against the background of bacterial and viral infections. With the development of diseases such as rheumatoid arthritis, SLE, scleroderma, Sjögren's disease, periarteritis nodosa and thrombocytopenic purpura, a high titer of antibodies to phospholipids is found in the blood of patients, which increases the likelihood of developing antiphospholipid syndrome.
Increased production of such antibodies is also observed in malignant neoplasms, taking certain medications (hormonal contraceptives, psychotropic substances), as well as after stopping anticoagulants. There is evidence of a genetic predisposition to the development of antiphospholipid syndrome.
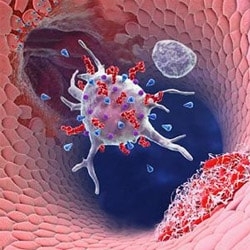
Phospholipids are subdivided into "neutral" and "negatively charged." Antiphospholipid antibodies react with phospholipids - lupus anticoagulant, beta2-glycoprotein-1-cofactor-dependent antiphospholipids. They interact with phospholipids of cell membranes of vascular endothelium, neutrophils and platelets. As a result, antibodies disrupt hemostasis and provoke a tendency to hypercoagulability.
How can antiphospholipid syndrome manifest itself? Damage to systems in APS
Antiphospholipid syndrome is considered to be a thrombotic vasculopathy of autoimmune origin. At the same time, the process can be localized in vessels of different caliber and location, which makes the clinical picture very diverse - from obstetric pathology to venous and arterial thrombosis, as well as cardiovascular, skin, neurological and hematological disorders.
 The most common manifestations of antiphospholipid syndrome are venous thrombosis, thrombosis of deep and superficial veins of the lower extremities. Patients with this syndrome are prone to episodes of PE, superior vena cava syndrome, pulmonary hypertension, adrenal insufficiency, and Budd-Chiari syndrome. With APS, thrombosis of venous vessels develop much more often than arterial ones. Arterial thrombosis is presented in the form of thrombosis of the cerebral arteries, which are manifested by ischemic attacks, as well as ischemic strokes.
The most common manifestations of antiphospholipid syndrome are venous thrombosis, thrombosis of deep and superficial veins of the lower extremities. Patients with this syndrome are prone to episodes of PE, superior vena cava syndrome, pulmonary hypertension, adrenal insufficiency, and Budd-Chiari syndrome. With APS, thrombosis of venous vessels develop much more often than arterial ones. Arterial thrombosis is presented in the form of thrombosis of the cerebral arteries, which are manifested by ischemic attacks, as well as ischemic strokes.
Which systems are more often affected in antiphospholipid syndrome?
- The cardiovascular system is affected by the development of myocardial infarction, arterial hypertension, cardiomyopathy against the background of ischemic disorders and the formation of intracardiac thrombosis. The valves of the heart are also affected, which is manifested by regurgitation and stenosis of the valves. If APS is suspected with cardiac manifestations, it is important to differentiate between infective endocarditis and cardiac myxoma.
- Proteinuria may occur if the kidneys are affected.
- Gastrointestinal tract lesions are represented by the development of gastrointestinal bleeding, mesenteric vascular occlusion, portal hypertension and hepatomegaly.
- The skin and soft tissues are affected with the formation of palmar and plantar erythema, trophic ulcers and livedo reticularis.
- Thrombocytopenia and hemolytic anemia are observed in the blood with antiphospholipid syndrome.
- In women of reproductive age, antiphospholipid cider is manifested by obstetric pathology – spontaneous abortions at different periods and intrauterine growth retardation, premature birth.

How to establish and confirm the diagnosis of antiphospholipid syndrome?
If you suspect antiphospholipid syndrome, you need to carefully examine the patient. Confirmation of the diagnosis is based on the detection of titers of antibodies to cardiolipin of the IgG / IgM class and lupus anticoagulant in the blood plasma. The diagnosis is considered confirmed if a positive test is obtained twice within 6 weeks. The diagnosis is valid in the presence of at least one laboratory and one clinical symptom. If APS is detected in a pregnant woman, the issue of her hospitalization and medical supervision is decided.
The main goal of therapy for the syndrome is to prevent thromboembolic complications. For this purpose, indirect and direct anticoagulants, antiplatelet agents are prescribed. In severe cases, glucocorticoids and a plasmapheresis session are indicated.







Add a comment