Scarring is a side effect of most surgical procedures, as well as many laser procedures. Although the scars themselves usually do not pose any threat to health, however, patients are often concerned about the appearance of the scar, especially when localized in open areas of the body. Laser medicine offers the possibility of scar correction without side effects or relapses.
 Vladimir Alexandrovich Tsepkolenko
Vladimir Alexandrovich Tsepkolenko
MD, Professor, Honored Doctor of Ukraine,
President of the Ukrainian Society of Aesthetic
Medicine, General Director of the Ukrainian
Institute of Plastic Surgery
and aesthetic medicine "Virtus"
It is generally accepted to classify scars into normotrophic, atrophic, hypertrophic, keloid.
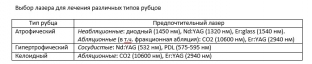
The following factors are important to determine the laser parameters and the minimum required number of treatments: color, texture and structure of the scar, as well as previous treatment experience (Table 5).
It is necessary to take into account the age of the scar, the type of impact that led to its formation, and the duration of the formation. Scars that have existed for less than one year are usually more erythematous than those that have existed for a long time. Although fresh scars can be easily corrected with a vascular pulsed laser, they usually decrease on their own, organized within a year, which eliminates the need for any additional treatment. However, treatment is strongly recommended when the scar worsens to prevent its pathological growth.
It is also important to know if the scar has been treated before, as the development of additional fibrosis with unsuccessful removal attempts significantly complicates the treatment. Atrophic scars previously treated with dermabrasion may not respond well to CO2 laser resurfacing due to subsequent tissue thickening.
Laser treatment of atrophic scars
Ablative skin resurfacing. Resurfacing with CO2 and Er:YAG lasers (8-10 J/cm2) of atrophic scars of moderate severity can improve their appearance and skin elasticity by 50-80% (Fig. 2.5-24).
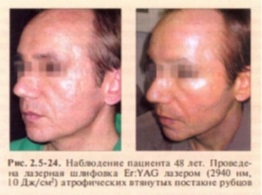
Collagen regeneration followed by clinical smoothing of the scar occurs within 12-18 months after the procedure, so re-treatment should be carried out no earlier than one year in order to accurately assess clinical improvements.
Non-ablative laser skin resurfacing (Nd:YAG, 1320nm; diode, 1450nm) has become widespread due to a significantly lower risk of side effects than ablative resurfacing. The radiation of these lasers penetrates the skin quite deeply, without severe thermal damage to the dermis and epidermis.
It is recommended to carry out three consecutive applications with an interval of one month. The greatest degree of improvement (40-50%) occurs approximately 3-6 months after the last treatment.
Pulsed vascular lasers (Nd:YAG, 532 nm; PDL, 575-595 nm, etc.) are used to reduce the vascularization of scar tissue, which contributes to the disappearance of hyperemia of atrophic scars and improve their appearance.
In hypertrophic and keloid scars, vascular coagulation accelerates the maturation of scar tissue in order to prepare them for subsequent vaporization.
Although the use of non-ablative techniques promotes the resolution of atrophic scars with minimal side effects, the degree of clinical improvement is significantly inferior to laser resurfacing. Therefore, in each case, it is necessary to choose the most appropriate method of treatment.
Fractional laser ablation achieves greater clinical improvement than non-ablative laser skin resurfacing while significantly reducing the postoperative period compared to ablative resurfacing. Produced with appropriate CO2 and Er:YAG lasers.
Fractional ablation is mainly used in the treatment of combined types of scars: a combination of atrophic and hypertrophic scars, as well as in the treatment of stretch marks. It should be noted that the treatment of scars with fractional laser ablation requires more procedures compared to ablative technologies.
Laser treatment of hypertrophic scars and keloids
The treatment of scars with a pulsed vascular laser leads to a significant reduction in erythema, restoration of elasticity and reduction in the size of the scar. Clinical observations are confirmed by structural analysis of the skin surface, measurements of scar height and elasticity indices. If scarring is accompanied by itching, oral antihistamines may be needed, but vascular laser treatment of scars can also help relieve symptoms.
While hypertrophic scars usually show significant improvement after vascular laser treatment, similar clinical results may require simultaneous injection of corticosteroids (diprospan no more than 1 ml per treatment) to achieve similar clinical results in the treatment of dense keloids. Additional injections of corticosteroids after laser treatment do not lead to a significant improvement in clinical results and should only be used for the most pronounced hypertrophic scars (Fig. 2.5-25).

It is recommended to treat the entire surface of the scar with non-overlapping laser pulses with a radiation energy density of 4.5-7 J/cm2. When treating scars in sensitive areas (the anterior surface of the chest) and in patients with IV and higher Fitzpatrick skin phototypes, the energy density should be reduced by 0.5-1 J/cm2 or more. During laser treatment, patients experience a tingling sensation, and for some time (up to 30 minutes) after treatment, there is a slight local increase in skin temperature.
Removal of keloids with a CO2 laser is less traumatic than excision with a scalpel, which has a high percentage of re-identification of keloids (50-70%).
Pre-treatment of keloids with a vascular laser and diprospan injections followed by CO2 laser vaporization is the optimal algorithm for the treatment of keloid scars, minimizing the likelihood of recurrence.
In the treatment of hypertrophic and keloid scars of moderate to severe scarring, resurfacing is used to remove abnormal tissue, which stimulates the synthesis of new collagen and elastin in the treated area and surrounding tissues. In the treatment of such scars, primary treatment with a vascular laser can be recommended in order to reduce the vascularization of scar tissue. After some time (6-10 weeks), the surface of the scar is resurfaced with an ablative laser, which gives a relatively acceptable result. If necessary, another procedure can be performed after at least a year.
Clinical guidelines:
- Hypertrophic or keloid scars are best treated with a vascular laser at two-month or longer intervals to maximize tissue healing;
- do not wait for purpura to appear during processing, as it is not the final purpose of the processing;
- ablative vaporization is most effective in the treatment of moderate to severe atrophic scars;
- mild to moderate atrophic scars respond well to non-ablative laser treatment;
- The final result of the scar correction is only assessed a few months after the completion of the series of treatments.
Laser scar treatment complications and their correction
Pulsed vascular lasers (Nd:YAG, 532 nm; PDL, 575-595 nm)
After treatment of scars with a vascular laser, hyperemia and edema persist for 2-3 days. Strict sun protection is required between treatments to avoid stimulating pigment synthesis in the treated areas. Treatments are usually done at 6-8 week intervals, however longer intervals between treatments may be needed for scars in long-healing areas (e.g. limbs).
Ablative laser skin resurfacing
Expected side effects immediately after treatment include significant erythema, edema, serous discharge. Erythema usually resolves on its own and does not require special treatment, its degree is proportional to the depth of ablation. Other possible complications include acne, sebaceous cysts (milium), and dyspigmentation. Short-term hyperpigmentation is the main side effect, but it resolves on its own in 1-2 months. The attachment of a secondary infection and the development of inflammation can lead to repeated rough scarring.
Fractional photothermolysis
Some of the expected complications associated with any laser treatment are redness and swelling. To treat these complications, preparations containing the regenerant dexpanthenol are used: panthenol, bepanthen, etc. in various forms of release, as well as irrigation of the treatment area with thermal water. Usually these complications resolve within 3-5 days.
To be continued.







Add a comment