The role of microbial biofilms in the development of adverse reactions after injections of dermal fillers has recently received more and more attention. Nodules, abscesses, delayed reactions, vascular damage, and infections are rare after these types of procedures, but do occur with long-acting dermal fillers made entirely or partly of non-absorbable polymers and may not resolve for months.
Negative culture results and lack of reliable identification of pathogenic bacteria – the reasons why such adverse events were previously attributed to allergic reactions. However, it is now believed that some of these may be caused by or as a consequence of biofilm formation.
- What is microbial biofilm
- How microbial biofilms are formed: the main steps
- Factors that increase the risk of microbial biofilm formation after fillers are injected
- How to prevent microbial biofilm formation
- Diagnosis of microbial biofilm: how to identify the problem
- Available treatments for microbial biofilm
What is microbial biofilm
Microbial biofilm – it is a collection of microorganisms (bacteria, protozoa, algae, fungi, yeast, etc.) that are physically interconnected. They produce an extracellular matrix containing many different types of extracellular polymeric substances, such as polysaccharides, proteins, etc. These surface microbial communities can form in any environment and are irreversibly attached (i.e., cannot be removed by light mechanical action) to living and non-living surfaces. .
Biofilms typically form on solid surfaces that are immersed in or exposed to water. In the human body, many chronic infections can be associated with a microbial biofilm that forms on surfaces:
- implants;
- tissue fillers;
- orthopedic implants;
- artificial heart valves;
- contact lenses;
- catheters;
- teeth.
This population of bacteria becomes resistant to the body's defenses, high doses of antibiotics, and is often not identified by culture, which complicates the treatment process and increases the likelihood of relapses. In addition, planktonic bacteria from the biofilm can enter the surrounding tissues or the bloodstream.
The following factors are thought to provide a layered defense that allows biofilms to become resistant to antibiotics:
- insufficient penetration of antibiotics;
- deceleration of the metabolism and growth of the microorganism;
- adaptive stress responses.
The biofilm becomes resistant to host defenses, high doses of antibiotics, and is often not identified by culture, making treatment more difficult and more likely to relapse. How microbial biofilms are formed: main steps
There are 4 main stages in the formation of microbial biofilms:
attachment of bacteria to surfaces;
- microcolony formation;
- biofilm maturation;
- variance. Free floating bacteria can attach to surfaces and become sessile. As a rule, biofilms form quickly, microcolonies can be detected as early as 8-10 hours after infection. Biofilm bacteria produce polymeric substances that form the basis for maintaining the integrity of its structure.
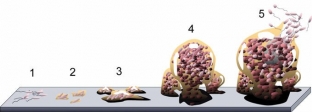 As the biofilm grows, bacterial resistance to antimicrobials increases and the immune system's effect on microorganisms is limited. As a rule, biofilms are located in an inactive, "dormant" state, however, under the influence of external trigger factors, they can be activated.
As the biofilm grows, bacterial resistance to antimicrobials increases and the immune system's effect on microorganisms is limited. As a rule, biofilms are located in an inactive, "dormant" state, however, under the influence of external trigger factors, they can be activated.
Interference with the biofilm's local environment, such as trauma, further injections, hematogenous infections, or medical procedures, can result in the following:
local sluggish infection;
- abscesses;
- local bumps;
- granuloma due to foreign body ;
- nodules; systemic infection. Factors that increase the risk of microbial biofilm formation after fillers are injected
Long-term use of fillers is associated with an increased risk of microbial biofilm formation, since "dormant" biofilm can be activated during repeated procedures. Other factors that may contribute to biofilm formation:
surface area of the product: the larger it is, the more space for bacteria to attach and colonize;
product duration;
- Incorrect injection technique (insufficient sterility). Some authors argue that the likelihood of biofilm formation depends on the filler used: resorbable products have a lower risk of long-term or late complications. However, further research is required to confirm or refute this theory.
How can microbial biofilm formation be prevented A complete patient history should include information on coagulopathy, compromised immune defenses, previous infections, or any existing infections in the treated area. In addition, it is necessary to find out if the patient has had tissue fillers or implants installed before. Infections in the treated or nearby area can escalate and cause complications. In this case, infecting organisms can colonize the area of implantation of the filler.
It is recommended to treat infectious diseases before installing dermal fillers, such as:
sinusitis;
periodontal disease;
- ENT infections;
- tooth abscesses.
- It is important to consider factors related to the patient, the product and the technique of administration to prevent adverse reactions.
Compliance with hygiene rules aimed at preventing microorganisms from attaching to the surface and the formation of a microbial biofilm is very important to prevent these types of complications. Therefore, it is necessary to adhere to a standardized procedure for the introduction of fillers and work with drugs.Aseptic technique is recommended when injecting dermal fillers. Skin disinfection, method and choice of disinfectant solution are also of great importance in the successful prevention of biofilm formation: alcohol antiseptics (chlorhexidine, povidone-iodine) are most effective.
In addition, it is recommended to use small-gauge needles whenever possible and to minimize
skin lesions.
Diagnosis of microbial biofilm: how to determine if there is a problem A complete patient history is required to diagnose any adverse reactions. A biopsy of the target area will help identify the microbial biofilm.
Recent studies have performed
in
situ
fluorescence hybridization, which have shown bacteria in the majority of culture-negative biopsies. Therefore, the cultural diagnostic method in the case of biofilms is not effective. DNA pyrosequencing and PCR testing of bacterial protein can be used to identify bacterial components of a biofilm. Accurate identification of causative organisms can minimize the potential for the development of resistant pathogens and improve the chances of successful treatment.
Available treatments for microbial biofilm In most cases, removal of the colonized implant and/or surgical excision of the infected tissue may be the only way to eradicate the biofilm-associated infection. Non-invasive treatments – antibiotics, steroids and 5-fluorouracil – only effective until a microbial biofilm is formed.
Antibiotics and drainage may be effective in suppressing active infection, but complete regression without removal of the implant and biofilm is extremely rare.
Cassuto et al. have used lithium triborate diode lasers at 532 nm and 808 nm to treat granulomatous and cystic lesions and report full or partial efficacy of this method. Mechanism of action – melting of tissue, filler and inflammatory cells with their subsequent removal through the holes. In addition, the authors suggest that the heat of the laser radiation (65-70
o
C) most likely kills the bacteria in the biofilm and melts the microparticles.
Read also: Bacterial biofilms after filler injections: a guide to action for cosmetologists
An in vitro study by Pecharki et al. showed that hyaluronidase promotes the separation of
Streptococcus
intermedius and effectively destroys bacterial biofilms. Acute infection must be successfully treated before removal/destruction of the dermal filler. Diagnosis and effective treatment of biofilms – important tasks of the esthetician, who must not only understand the potential complications associated with the formation of microbial biofilms, but also take timely measures to prevent the formation, diagnosis and treatment of biofilms.







Add a comment