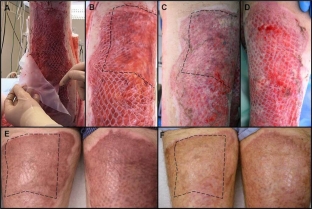
The use of skin grafts in modern plastic surgery opens up great opportunities for the reconstruction of damaged skin areas. Not all wounds can be closed by suturing them, since very often the size of the defect is so large that the edges of the wound simply cannot be reduced. In such cases, skin graft transplantation is the optimal treatment option. But the successful operation – this is not always a guarantee of a good effect. Skin graft necrosis can occur in the postoperative period and proper care during this time is the best method of preventing graft rejection.
Prevention of transplant rejection in the postoperative period
Postoperative period – this is the period of time after the operation and until the complete healing of the damaged area. At this time, the patient requires especially careful care, which is necessary both to improve his general condition and eliminate pain, and to control and maintain the entire body in the recovery period. Prevention of graft rejection after transplantation at this time implies proper postoperative care. It includes the removal of hematomas and seromas that may form between the graft and the recipient bed, care of the infected graft, and some other manipulations.
Prevention of transplant rejection:
- removal of seromas and hematomas to prevent graft rejection;
- prevention of graft rejection in the development of an infectious process;
- immobilization of the graft to prevent the development of its contraction.
Removal of seromas and hematomas to prevent graft rejection
Seromas and hematomas in the postoperative period can form between the recipient bed and the skin graft, preventing its vascularization and contributing to the development of necrotic processes. To prevent graft rejection, it is necessary to remove the resulting hematomas and seromas in a timely manner. If there are suspicions about the possibility of fluid accumulation between the graft and the recipient bed – on the 2nd day after the operation, an audit of this area is performed and the liquid is evacuated until it stops accumulating. The fluid is removed by pressing on the graft with sterile gauze balls, and the resulting clots are removed with tweezers.
Prevention of graft rejection in the development of an infectious process
In the postoperative period after any of the surgical interventions, there is a possibility of developing an infectious process. The following signs indicate the development of infection under the graft:
- increase in body temperature to subfebrile values, often 3-4 days after surgery;
- unpleasant odor in the graft area;
- redness around the edges of the graft a few days after surgery;
- increased pain at the graft site.
Prevention of graft rejection in case of infection includes mechanical removal of necrotic tissue, abundant washing of the wound with saline, as well as the appointment of antibiotic therapy in accordance with the infectious agent. Significantly increases the survival rate of split skin grafts hyperbaric oxygenation.

Immobilization of the graft to prevent the development of its contraction
In the postoperative period, it is important to pay sufficient attention to the immobilization of the skin graft to prevent the development of its contraction. As is known, absolutely all skin grafts undergo this process to the extent that maturing scar tissue contracts between the recipient bed and the skin graft. This process begins about 10 days after surgery and continues for about six months. Thin split grafts are especially subject to pronounced contraction on mobile and concave body surfaces, and to a much lesser extent – in fixed and convex areas. Full-thickness grafts are practically not subject to contraction.









Add a comment