Over the past decade, dermal filler injections have become one of the most popular ways to restore lost facial soft tissue volume and rejuvenate it. For the most part, filler injections are absolutely safe, however, no one is immune from the unwanted effects of beauty injections, and reports of complications after fillers, including cases of temporary or permanent loss of vision, skin necrosis or scarring, regularly appear in the press. .
Let's consider the mechanism of occurrence of complications after the introduction of fillers from the point of view of the anatomical structure of the human face, as well as ways to avoid or prevent the development of adverse events.
- Anatomical structure of the face
- Location of blood vessels in hazardous areas
- Possible Complications: Symptoms and Management
- Principles for the safe administration of
fillers in hazardous areas Anatomical structure of the face
The most serious complications after the introduction of fillers include:
unilateral or bilateral visual impairment or blindness;
- skin necrosis;
- cerebrovascular disorders.
- The dermal fillers most commonly associated with complications include hyaluronic acid, calcium hydroxyapatite, polymethyl methacrylate, polylactic acid, silicone, and adipose tissue.
- The key to understanding the causes of various complications after the introduction of fillers is a good knowledge of the structure of the vascular system of the face. In general terms, in the anatomical structure of the human face, 5 layers can be distinguished:
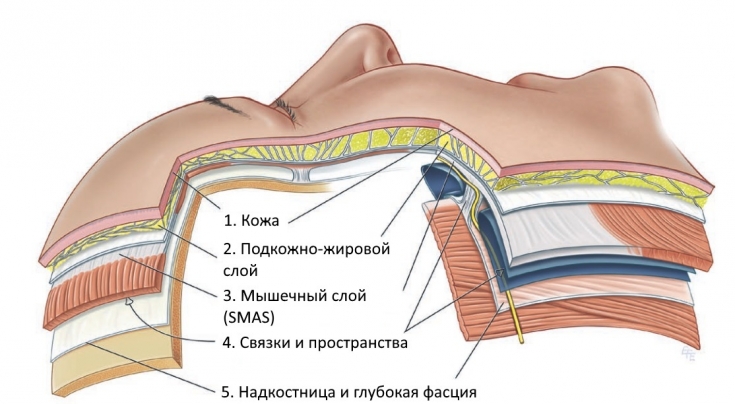
- Subcutaneous fat deposits
- Facial muscles and SMAS
- The system of blood vessels
- Skull
 You should also take into account all the procedures and operations that the patient has undergone before, as they could affect the anatomical structure of the face and be a factor in the increased risk of undesirable consequences of
You should also take into account all the procedures and operations that the patient has undergone before, as they could affect the anatomical structure of the face and be a factor in the increased risk of undesirable consequences of
filler injections. Location of blood vessels in hazardous areas
The most
dangerous complicationassociated with dermal fillers is venous or arterial occlusion, which can lead to ischemia and subsequent skin necrosis and/or loss of vision. All of these phenomena are highly undesirable and require immediate medical attention. Arterial occlusion can lead to the formation of ulcers, scars, and occlusion of the ophthalmic artery – to loss of vision.
Arterial or venous occlusion may be caused by the injection of a filler directly into a vein/artery, damage to a blood vessel or external pressure exerted on it by the injected filler or edema. In general, vascular occlusion and necrosis are considered rare complications.
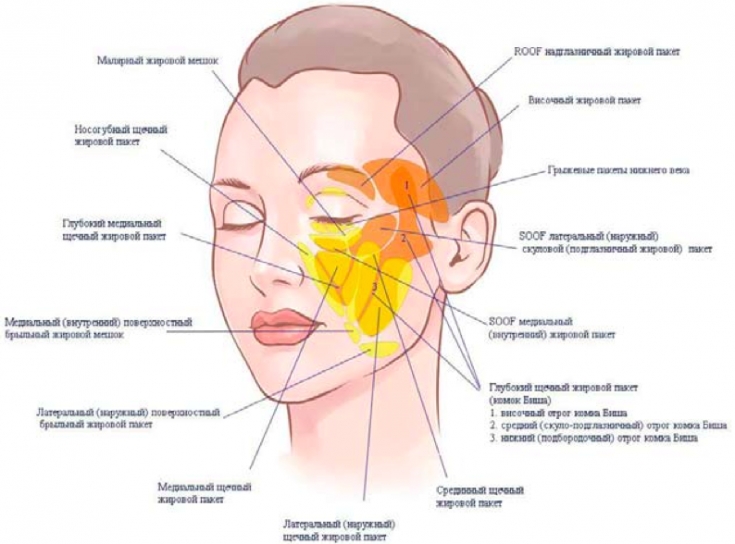
 The main danger zones of the face, which should be avoided during the introduction of fillers. In the cheek area it is:
The main danger zones of the face, which should be avoided during the introduction of fillers. In the cheek area it is:
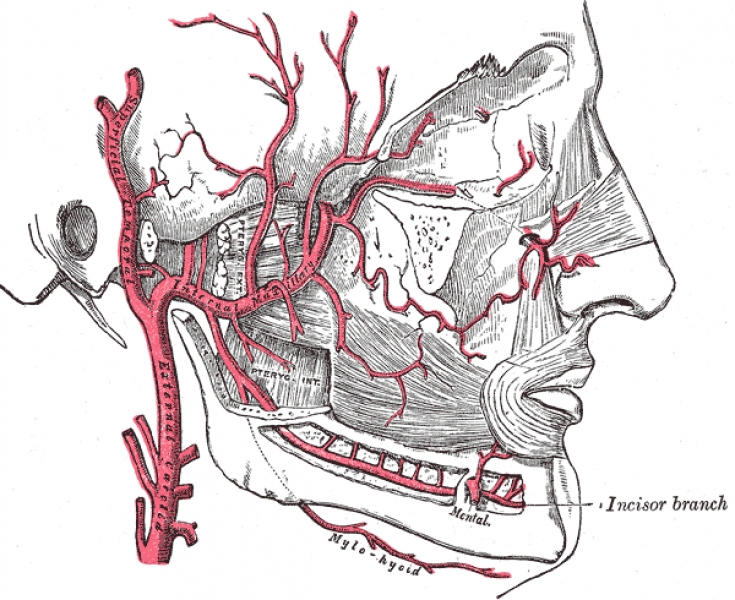
facial artery;
- transverse facial artery;
- buccal branch of maxillary artery;
- infraorbital artery;
- zygomatic branch of the buccal artery.
- In the area of the glabella, due to the small diameter of the vessels and insufficient collateral circulation, the introduction of fillers should be done with extreme caution. Here the danger zones are:
frontal artery;
- supraorbital artery.
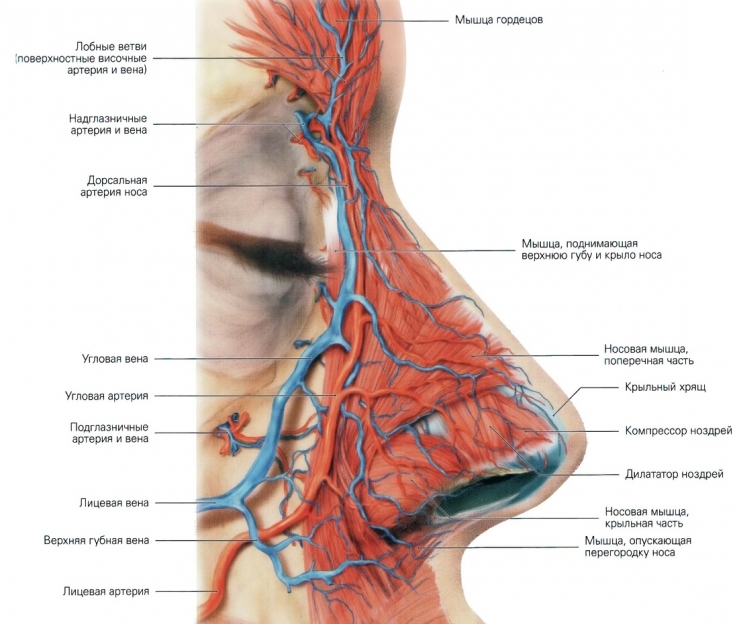
- Hazardous areas in the nasal area include:
external nasal artery;
- angular artery.
 In the perioral zone it is:
In the perioral zone it is:
superior labial artery;
- inferior labial artery.
- In the temple area, fillers are injected with care, avoiding getting into the superficial temporal artery, its posterior parietal and
anterior frontal branches. Possible Complications: Symptoms and Treatment
Skin discoloration immediately after filler injection indicates vascular ischemia. Symptoms of arterial or venous occlusion, which can lead to skin necrosis, are discoloration of the skin or its darkening (to gray-blue shades), ecchymosis, erythema reticularis, and severe pain at the injection site.
In case of vascular occlusion or impending necrosis, the main goal is to stimulate blood flow in the affected area.
Principles of emergency care for vascular occlusion
immediate application of a warm compress,
- Massage the affected area to dilate the blood vessels and disperse the injected drug,
- taking aspirin,
- use of topical vasodilators
- hyaluronidase injection (in case of hyaluronic acid fillers),
- corticosteroid injection (anti-inflammatory/immunomodulatory),
- taking antibiotics,
- taking antiviral drugs (in case of threat of necrosis in the perioral area).
- It is also possible to use hyperbaric oxygen therapy and laser procedures 3 months after the filler injection.
Cases of retinal artery occlusion are extremely rare and very dangerous. Symptoms of possible loss of vision are sharp pain in the area of the affected eye immediately after the injection of the filler, blurred vision, ptosis, headache, dizziness, nausea, ophthalmoplegia.
Read also:The Dublin Protocol for Treatment of Complications After Fillers. In the event of retinal artery occlusion, visual loss is usually irreversible. The best way to prevent this extremely undesirable phenomenon is to avoid dangerous areas when introducing fillers, especially – in the region of the glabella, forehead and upper part of the
nasolabial folds. Principles for the safe administration of fillers in hazardous areas
In rare, but still probable, cases of vascular occlusion and subsequent necrosis and/or loss of vision after fillers, emergency medical attention is essential.
Sudden sharp pain and/or discoloration of the skin are warning signs of vascular occlusion, ischemia and impending necrosis. To reduce the likelihood of undesirable consequences of this nature, it is recommended to follow the rules.
Read also:A Quick Guide to Injectable Filler Techniques. Rules for the safe administration of fillers
inject filler in small doses,
- do not apply anesthesia (including drugs containing epinephrine) near the vascular bundles, so as not to cause vascular spasm,
- Avoid epinephrine to be able to quickly identify the cause of skin discoloration,
- Use a small needle to ensure that the filler enters the tissues with minimal doses,
- Use biodegradable fillers (e.g. hyaluronidase stimulates rapid degradation of hyaluronic acid fillers),
- when inserting the filler with the finger of the non-dominant hand, block the adjacent blood vessel,
- introduce the filler into the upper and middle layers,
- assess the level of pain in the procedure,
- monitor for possible changes in skin color,
- in case of using non-biodegradable fillers, inject them in small doses and take into account their high viscosity.
3D Lift technique for inserting fillers into the nasolabial fold and middle third of the face. To prevent such a complication as vascular occlusion, I suggest using a simple and effective method - an aspiration test: after inserting the needle into the correction zone and before starting the drug delivery, it is necessary to carry out a slight reverse movement of the syringe piston. If there is no blood, you can start injecting the drug. This test allows you to exclude the drug from entering the vascular bed.
More interesting videos on our





