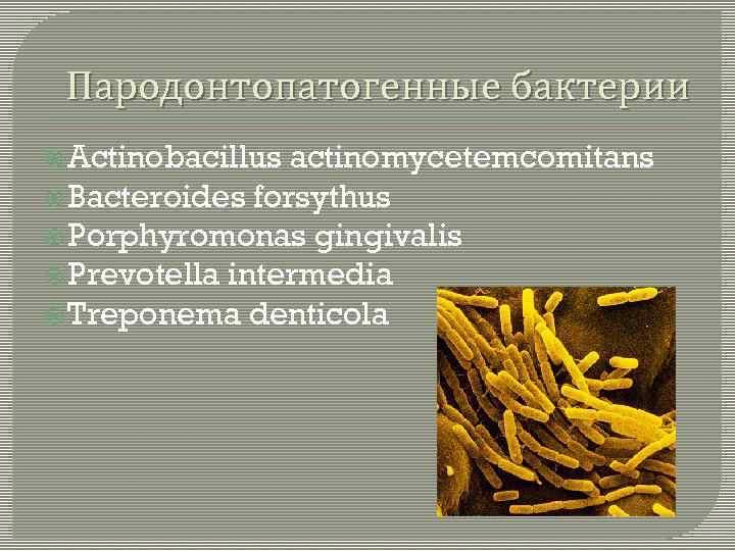
Interest in periodontitis as a potential risk factor for the development of atherosclerosis and its complications is due to the fact that the global prevalence of periodontal disease is significant and entails an inflammatory process in the body. Many studies have analyzed the potential impact of Porphyromonas gingivalis, the main pathogen of periodontitis, on overall health.
The article on ester-portal.com provides research data confirming the role of periodontopathogenic bacteria in the development of atherosclerosis and cardiovascular diseases.
- The mechanism of atherosclerosis and the contribution of periodontopathogenic bacteria
- Methods and results of the study of periodontopathogenic bacteria in the development of atherosclerosis and cardiovascular disorders
- Conclusions
The mechanism of atherosclerosis and the contribution of periodontopathogenic bacteria
An important element in the prevention of atherosclerosis and its complications is the understanding of the pathomechanisms leading to damage to the walls of blood vessels.
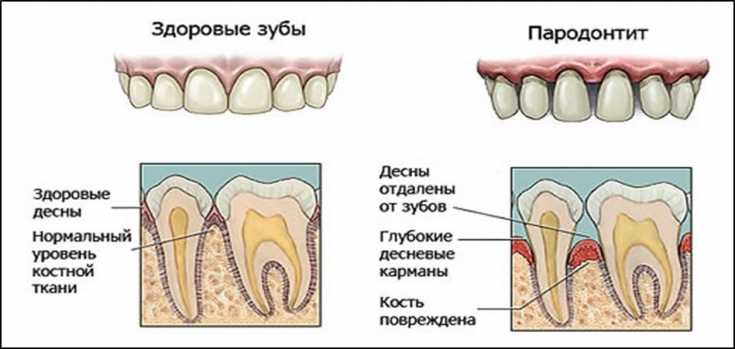
Porphyromonas gingivalis is a microorganism found in periodontal pockets and biofilm. The presence of this pathogen is associated with chronic periodontitis and an inflammatory reaction of the circular ligament of the tooth.
Read also: Warning factors that can detect atherosclerosis.
Research over the past two decades has shown that in addition to the usual risk factors leading to the development and progression of atherosclerotic plaques, the condition may also be the result of microorganisms, elevated levels of fibrinogen, C-reactive proteins and antibodies. On this basis The immune-inflammatory theory of atherosclerosis has been established, according to which atherosclerosis is a chronic immunofibroproliferative inflammatory response to factors that damage vascular endothelial cells.
A large amount of data proving the involvement of chronic inflammation in the pathogenesis of atherosclerosis and destabilization of atheromatous plaques in the arteries has forced many researchers to focus their attention on finding the cause of inflammation.
Follow us on Instagram!
Interest in periodontitis as a potential risk factor for the development of atherosclerosis and its complications is due to the fact that the global prevalence of periodontal disease is extremely high and, in addition, periodontitis can cause a chronic inflammatory response.
Mild forms of periodontal disease, including gingivitis, affect up to 70% of the general population, while approximately 10% to 15% of the population is affected by processes associated with the destruction of tissues supporting the tooth. Many studies since 1989 have analyzed the potential impact of Porphyromonas gingivalis, the main pathogen of periodontitis, on general health and especially in the context of cardiovascular problems.
In patients suffering from periodontitis with damage to the periodontal pocket, transient bacteremia not only occurs during medical procedures, but also during brushing and chewing.
The effect of P. gingivalis on the cardiovascular system indirectly virulence factors, so it not only becomes destructive to periodontal tissues, but can also cause general inflammation.
Read also: Myths about cholesterol.
The purpose of this study was to assess the condition of periodontal tissues in patients who were scheduled for surgery due to atherosclerosis and its complications.
Porphyromonas gingivalis DNA, a bacterium closely associated with periodontitis, has also been demonstrated in periodontal pockets, as well as in coronary and carotid atherosclerotic plaques, in patients with chronic periodontitis who were hospitalized and underwent surgery due to - for vascular diseases.
Methods and results of the study of periodontopathogenic bacteria in the development of atherosclerosis and cardiovascular disorders
The study population consisted of 91 patients (78 males and 13 females) treated at a cardiac surgery clinic or a vascular, general and transplant surgery clinic.
Presence of Porphyromonas gingivalis DNA in atherosclerosis plaques was determined by PCR. Bacterial DNA was detected in 21 of 91 (23%) vascular samples and 47 of 63 (74.6%) periodontal pocket samples.
Scientists also suggested that the presence of bacterial DNA in vessel walls does not prove the presence of live bacteria capable of invading cells and causing inflammation.
So they did a study using quantitative PCR and then labeled the tissues to be tested. Live bacteria Porphyromonas gingivalis and Aggregatibacter actinomycetemcomitans were present in samples of atheromatous plaques in endothelial cells. This study proved for the first time that the detected bacterial DNA was derived from living bacterial cells, because only living microorganisms are able to enter cells other than phagocytes.
Read also: Tweaking gums: periodontitis treatment.
In this study, Porphyromonas gingivalis DNA was not found in periodontal pockets in 6 patients, but it was detected in samples from blood vessels.
Read also: Dental tissue engineering using stem cells
This situation can be explained by the fact that in chronic periodontitis there are short periods of exacerbation of inflammation and long periods of remission. In addition, most of the patients were elderly and had lost some teeth ("elderly" is defined as 65 years of age, according to the contractual age limit accepted in most developed countries).
Conclusions
The conclusion is therefore that it is possible that established periodontal pathogens present in the sublingual space and in the biofilm could easily find their way into the arteries.
Consequently, current periodontitis may be one of the factors affecting patients at risk for atherosclerosis and related diseases. For this reason, periodontal care should be considered a necessity for all patients at risk for vascular and cardiac disorders.
Source: "US national library of Medicine National Institutes of health"







Add a comment