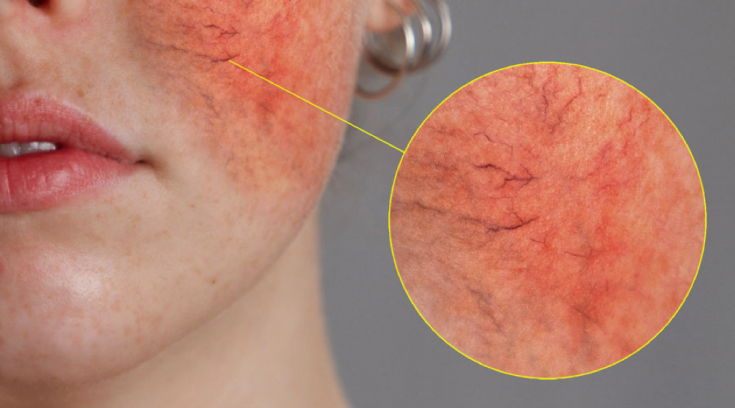
Rosacea – a chronic inflammatory skin disease that mainly affects the central part of the face. The disease manifests itself with a number of symptoms that can appear simultaneously or separately and change over time. These include: erythema – persistent redness, which is characterized by periodic exacerbations, is considered a hallmark of rosacea; papules and pustules; telangiectasia; phymatous changes; painful tingling or burning of the skin. Some patients also develop eye symptoms of rosacea. In an article on estet-portal.com, Drs. Sandra Marchese Johnson, Andrew Berg and Chelsea Barr discuss modern treatments for rosacea using topical drugs,
- Current approaches to the treatment of rosacea
- Topical treatment of rosacea in the presence of erythema, papules and pustules
- Oral Therapy for Moderate or Severe Rosacea
- Physical therapy for the treatment of telangiectasia and phymatous changes
- The role of proper skin care and lifestylelife in the treatment of rosacea
Patients with rosacea usually present with more than one symptom
at oncesuch as persistent erythema and pustules.
Furthermore, erythema and rosacea lesions are thought to share inflammatory characteristics, including inflammatory cell migration. Persistent erythema may be the first sign of inflammation and therefore requires attention.According to the consensus recommendations, multiple symptoms of rosacea
are best treated with combination therapy with the use of medicamentous, topical preparations and physical methods of influence.
Topical therapy for rosacea in the presence of erythema, papules and pustulesThe following agents are FDA approved for topical treatment of rosacea:
- Ivermectin cream 1% – with inflammatory formations;
- metronidazole cream 0.75% (twice a day) – with inflammatory formations;
- metronilazole gel 1% (daily) – with inflammatory formations;
- azelaic acid 15% gel or foam (twice daily) – with inflammatory formations;
- brimonidine gel 0.33% – with erythema;
- Oxymetazoline Cream 1% – with erythema.
Topical therapy for papules and pustules in rosacea
- Ivermectin
ophthalmic rosacea, including foreign body sensation, burning and photosensitivity.
- Metronidazole

Metronidazole is well tolerated with moderate adverse events such as pruritus, irritation and dry skin.
- Azelaic acid
Read also: Botulinum toxin: treatment of pathological scars and rosacea
Topical treatment of erythema in rosacea
Redness – typical symptom of rosacea – can be presented in various forms. Depending on the cause of the symptom, approaches to the treatment of erythema may vary.
Redness may be due to:
- vasodilation,
- anomalies of superficial skin vessels, including telangiectasia;
- presence of papules or pustules;
- inflammation caused by impaired skin barrier function.
Alpha-adrenergic receptor agonists
In August 2013, the FDA approved brimonidine 0.33% gel for the treatment of persistent facial erythema in rosacea, and in 2017 – oxymetazoline cream 1%.Brimonidine acts predominantly on alpha-2 receptors, while oxymetazoline – on alpha-1 receptors. Theoretically, clinical activity depends on the activity of receptors, however, such a relationship has not yet been proven.
Brimonidine is used in the treatment of erythema in rosacea because the substance causes vasoconstriction and may have anti-inflammatory effects. The drug begins to act quickly, the effect lasts about 12 hours.
You may also be interested in: Assessing the depth of vascular lesions in rosacea
Oxymetazoline also works for about 12 hours, but the effectcomes on more slowly than with brominidine.
Oral therapy for moderate to severe rosaceaPerioral medications may be indicated for moderate to severe rosacea. They are often prescribed for ophthalmic rosacea.
Antibiotics
While tetracyclines and azithromycin are used forthe treatment of rosacea off-label, only the subantimicrobial dose of doxycycline (40mg). The efficacy of antibiotics in the treatment of rosacea is thought to be more anti-inflammatory than antimicrobial. This explains the effect of subantimicrobial doses of doxycycline – the drug has an anti-inflammatory effect in concentrations that are not sufficient to suppress bacterial activity.
Due to changing patterns of resistance, experts are moving away from using standard doses of antibiotics to treat rosacea.
If standard doses of antibiotics are prescribed for rosacea, the course should be limited and patients should be switched to topical therapy
as soon as improvement occurs. Physical therapy for the treatment of telangiectasia and phymatous changes
Physical therapies may be indicated for the treatment of telangiectasias and phymatous changes in rosacea.
Lasers andIPL-therapy demonstrate efficacy in the management of these symptoms of rosacea, but data are limited to a small sample.
– an important condition for effective control of chronic inflammatory skin disease. The patient must be made aware that lifestyle changes can significantly reduce the severity of rosacea symptoms. The role of proper skin care and lifestyle in the treatment of rosacea
Proper skin care for rosacea aims at:
recovery of the skin barrier;
- UV protection.
- The application of topical preparations to skin with impaired barrier function increases the risk of treatment intolerance.
Proper skin care – the most effective way to relieve dry skin and the discomfort of rosacea.
For rosacea, it is recommended to regularly use sunscreens with SPF 30 or higher, which provide broad spectrum protection against:
UVA;
- UVB;
- infrared radiation;
- blue light.
- It is also recommended to use light moisturizers and cleansers.
The role of home care in preventing the onset and exacerbation of couperosis in rosacea A wide range of treatment methods allows the doctor to create an individual treatment plan for rosacea for each patient and get excellent clinical results. Topical preparations form the
mainstay of rosaceatreatment and can be very effective in controlling acne and erythema, as well as itching, stinging and burning of the skin. Trigger avoidance and proper skin care greatly enhance the effectiveness of rosacea therapy.
Based onJ Clin Aesthet Dermatol
More interesting videos on our





