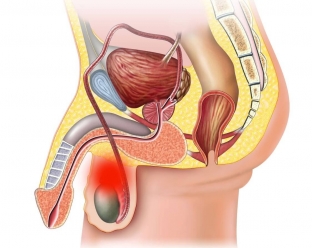
The seminal cyst of the testicle or its epididymis is called spermatocele. The cyst contains seminal fluid, spermatozoa, epithelial cells, fatty bodies and spermatocytes. Spermatocele is formed against the background of a violation of the process of secretion outflow from the epididymis with its accumulation in the excretory duct. Therefore, a pathological cavity is formed in the region of the head or tail of the epididymis and spermatic cord. Such a formation is defined by touch as a smooth, rounded, painless densely elastic formation, which is located in the scrotum above the testicle. Spermatocele can be acquired or congenital.
Main causes and clinical manifestations of spermatocele
Among all urological pathologies, spermatocele accounts for 7% of patients' visits to specialists. Spermatocele is benign in nature and manifests itself during the period of active and abrupt sexual changes that occur in adolescence and at the age of 40-50 years.
Congenital spermatocele is formed due to partial non-closure of the vaginal process of the peritoneum from the embryonic rudiments of Mullerian cells. What are the symptoms of spermatocele, read further on estet-portal.com. In the course of the spermatic cord and the epididymis, cavities remain that do not communicate with each other. A congenital spermatocele is usually small and contains no spermatozoa.
Against the background of diseases such as vesiculitis, epididymitis, deferentitis or orchitis, the ducts change, after which they cease to function due to obstruction. The seminal secret is unable to exit and overflows the duct. The wall of the duct is stretched, forming a cyst.
Acquired spermatocele appears after inflammatory processes or injuries of the scrotum. It can have content of different colors, one or more cameras.
Clinical symptoms of spermatocele development:
- In most cases, spermatoceles do not show symptoms, but slowly increase in size.
- No sexual dysfunction observed.
- A spherical mass is palpable in the scrotum.
- When the spermatocele reaches a large size, patients complain of discomfort in the scrotum, its enlargement, pain and heaviness during walking and sexual intercourse.
- Complications of spermatocele include suppuration and rupture of the seminal cyst.
Methods of diagnosis and aspects of treatment of spermatocele
History, examination and palpation reveal a large spermatocele. Diaphanoscopy and ultrasound of the scrotum allow you to quickly diagnose the condition. Diaphanoscopy is used to determine the nature of the formation in the scrotum by transilluminating it with rays of transmitted light. When the scrotum glows red, the presence of a spermatocele is suspected, since the liquid freely transmits light. Differential diagnosis is carried out with testicular cancer, dermoid cyst and hydrocele.
Spermatoceles of small size, which do not disturb the patient, do not require specific treatment. With an increase in the scrotum and the presence of a clinical picture of inflammation, the spermatocele is surgically excised.
After spermatocelectomy, it is recommended to apply a suspensorium for several days to maintain the scrotum. Also, after removing the spermatocele, it is recommended to apply ice to eliminate swelling. Less commonly, sclerotherapy and needle aspiration are used to treat spermatocele.






Add a comment