The use of biological therapy has expanded over the past decade far beyond primary autoimmune diseases. Indeed, a recent study using antibodies to interleukin-1 alpha and beta (in this case, canakinumab, a monoclonal antibody targeting interleukin-1β; IL-1β) demonstrated a reduction in the incidence of recurrent myocardial infarction, stroke and cardiovascular death. .
Psoriasis — it is a chronic inflammatory disease in which the use of biological agents is successful. Psoriasis is associated with an increased risk of myocardial infarction.
In the article estet-portal.com you can read in detail a study that examined the effect of biological therapy for psoriasis on the state of coronary plaques, including the volume of non-calcified coronary plaque and lipid-rich necrotic nucleus.
Biological therapy of psoriasis: impact on coronary artery atherosclerosis
The prospective observational study recruited 290 participants from January 1, 2013 to October 31, 2018, of whom 215 completed the one-year follow-up.
Severe psoriasis is associated with a more than 2-fold increased risk of myocardial infarction, with rates of coronary heart disease similar to type 2 diabetes.
Psoriasis treatment: experience with vitamin D
Psoriasis patients were middle-aged (mean — 50.5 years), mostly male (n = 70, 58%) with low Framingham cardiovascular risk (median 3) and severe dermatological pathology moderate to severe (median psoriasis area and severity index [mdash; PASI] equal to 8.6).
Psoriasis skin contains the cytokines IL-1.beta., interleukin-17 (IL-17) and tumor necrosis factor-.alpha. (TNF-α), which play an important role in early atherogenesis and plaque rupture.
Follow us on Facebook
Biological therapy for psoriasis is the future
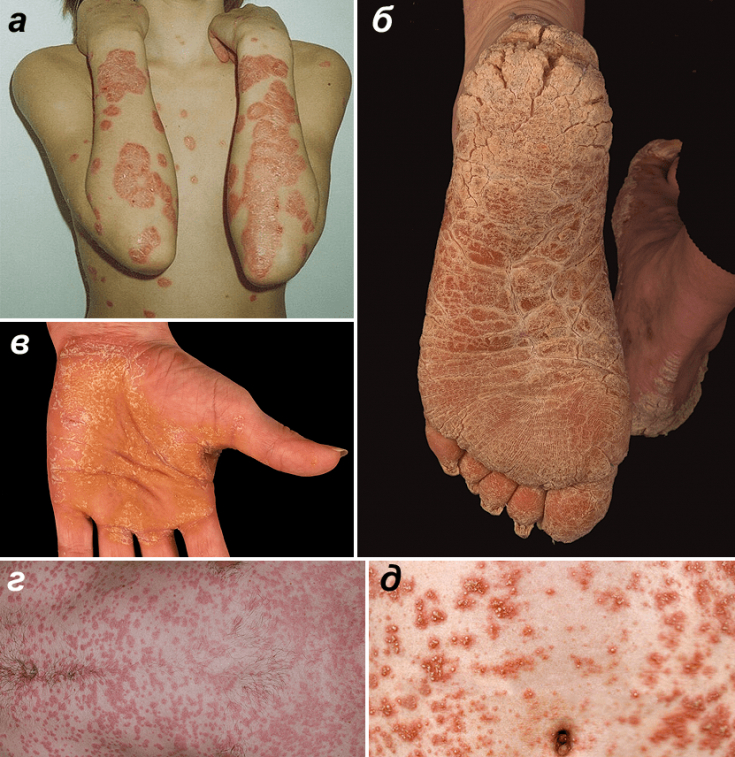
Figure 1. Forms of psoriasis. and — Vulgar psoriasis. Typical plaques on the skin of the extensor surface of the arms and on the chest. b — Psoriasis of the soles. in — Psoriasis of the palms. — Guttate psoriasis. d — Pustular psoriasis von Zumbusch.
Biological therapy was associated with a 6% reduction in non-calcified coronary plaque volume (P = 0.005), a reduction in necrotic core (P = 0.03), with no effect on fibrous load (P = 0.71). The reduction in non-calcified coronary plaque volume in the biologic group was significant compared to the slow progression of atherosclerosis in nonbiologic patients (-0.07 mm2 vs. 0.06 mm2, respectively; P = 0.02).
The authors demonstrated that biologic therapy for psoriasis was associated with a reduction in non-calcified coronary plaque volume and improved plaque morphology compared to those receiving non-biologic therapy. These data highlight the potential role of inflammatory suppression in cardiovascular disease.
The results of the study support the need to expand understanding of the potential effects of biologic therapy on the coronary vasculature.
Thank you for staying with estet-portal.com. Read other interesting articles in the "Experts" section. You may be interested in Psoriasis of the scalp: principles of diagnosis and treatment







Add a comment