(as «zaedy») – this is a pathological condition characterized by inflammation of the corners of the mouth and the formation of characteristic cracks, crusts and redness. The prevalence of angular cheilitis is 7 per 1000 persons, and the disease is more common in older people. Angular cheilitis is twice as common in men as in women.
Being a rather catchy and subjectively unpleasant phenomenon, angular cheilitis can create certain psychological and social difficulties for the patient.
In this article on estet-portal.com, read
about the factors that can lead to the development of angular cheilitis,as well as about modern approaches to the treatment of this condition, based on evidence-based medicine. Angular cheilitis etiology: infections, injuries, vitamin deficiencies
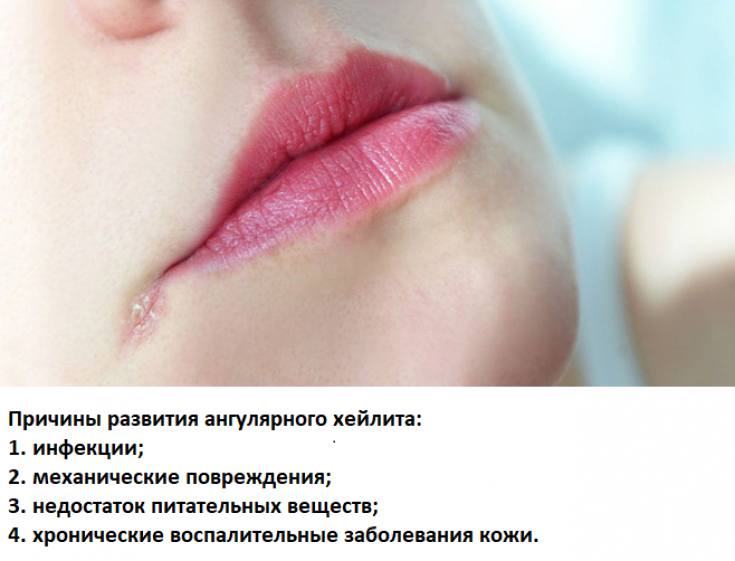
Various pathological conditions can lead to the development of angular cheilitis, among which four main groups should be distinguished.
Follow us on These include:1. Infections:
especially Candida albicans and Staphylococcus aureus, which can cause cheilitis either alone or together. Candida albicans is often identified as the cause of cheilitis in diabetic patients;
2. Mechanical factors:ill-fitting dentures, improper use of dental floss, dental trauma, and excessive salivation or, conversely, – xerostomia can lead to the development of maceration of the commissural epithelium;
3. Nutrient deficiencies, in particular proteins, B vitamins (B2, B3, B12), folic acid and zinc;
4. Chronic inflammatory skin diseases:atopic dermatitis, contact dermatitis.
What lips suffer from: meteorological cheilitis Pay attention to the tongue: characteristic mucosal changes
When examining a patient with angular cheilitis, it is important to pay attention to the condition of his tongue, changes in which are often observed as concomitant.
Pale color of the tongue, its smooth surface, as well as the presence of aphthous ulcers in the oral cavity may indicate an iron deficiency in the patient's body. At the same time, a glossy bright red tongue is characteristic of a lack of niacin, B12 or folic acid in the body.
A reddish-purple color of the tongue is quite specific for riboflavin deficiency.

Atopic cheilitis develops with poor oral hygiene Angular cheilitis: the feasibility of additional research methods
In most cases, angular cheilitis does not require additional research methods – the diagnosis is established clinically. Exceptions are conditions in which there is a lack of effectiveness from the treatment.
It may sometimes be necessary to examine samples of the oral mucosa (if the patient wears dentures from under them) and the nose for the presence of bacteriological and mycological cultures, but this is not a routine analysis performed for angular cheilitis.
A patient with frequently recurrent angular cheilitis should be advised by a physician to undergo HIV testing.
Defects of the red border of the lips: what is the danger of cheilitis Angular cheilitis treatment: antifungal ointments and nutrients
According to current international recommendations, specific therapy for angular cheilitis is the appointment of local antifungal agents (miconazole cream 2%).
Miconazole should be applied in a thin layer to the affected area in the morning and evening for 7-14 days. This drug also shows its effectiveness against gram-positive bacteria.
Pharmacological interactions of miconazole with drugs such as warfarin, phenytoin and productive sulfonylurea drugs should be taken into account – he is able to enhance their action.
Therefore, patients taking the above medications should be given topical nystatin instead of miconazole.
If the cause of the development of angular cheilitis – If this is a lack of nutrients, it is important to compensate for their deficiency by prescribing the patient a good diet and, if necessary, medications (for example, B vitamins). Before prescribing vitamins, it is important to make sure that the patient has a true deficiency.
In addition to etiotropic therapy, a patient with angular cheilitis should carefully monitor the state of oral hygiene. If he wears dentures – they must be removed at night and cleaned before each reuse.
Thank you for staying with estet-portal.com. Read other interesting articles in the "Dermatology" section. You may also be interested in
Vulnerable Mouths: Diagnosis and Treatment of Exfoliative Cheilitis







Add a comment