Back in 1880, a microbe was discovered in a woman suffering from osteomyelitis, to which Louis Pasteur gave the name – staphylococcus aureus It is he who triggers the onset of the disease known as osteomyelitis of the jaw – an infectious inflammatory disease that develops in the bone tissue of the maxillofacial region, developing into necrosis. The average age of the disease is 25-40 years. To diagnose this disease, an x-ray, a general examination, a hemogram are used. In surgical dentistry, this type of osteomyelitis occurs in chronic, acute, subacute forms, localized both in the upper and lower jaws.
reasons why a purulent process of bone tissue develops.
- Symptoms and stages of development of osteomyelitis of the jaw
- Causes of osteomyelitis of the jaw and diagnosis
- Preventive advice for osteomyelitis of the jaw
Osteomyelitis of the jaw – this is advanced periodontitis or periostitis, but whether this disease turns into a purulent process depends on the general condition of the body. Weak immunity and an unhealthy lifestyle increase the risk. elevated body temperature up to 39-40 degrees, it is difficult to get off;
• headache, feeling of loss of strength;
• pain sensations localized in the region of the diseased tooth, the pain passes to the adjacent organ (ears, eyes, nose);
• there is an unpleasant sensation when eating and chewing, it is more convenient to keep the mouth ajar;
• the infected tooth begins to wobble and affect others;
• gums bleed when pressed, swelling is present;
• lymph nodes increase, one side of the face swells.
Subscribe to our page on
Instagram!
The acute stage turns into a chronic form when it starts. The pain disappears, the temperature gradually subsides. A fistula filled with pus appears in the area of \u200b\u200bthe diseased jaw. On the part of the infected tooth, the cheek, tongue, and mucous membrane of the cheeks swell. There is a syndrome of Vincent – numbness of the chin and lips. The subacute stage appears 2-3 weeks after the first signs.
Inflammation of the tooth root: <
Causes of osteomyelitis of the jaw and diagnosis
The processes of putrefaction and infection are triggered by bacteria. When the bone tissue is affected by microorganisms, inflammation begins. Staphylococcus aureus and streptococcus are the causative agents of osteomyelitis of the jaw in 90% of cases. carious tooth, gum disease (75-80%); • the presence of an infection in the body (microbes enter the jaw through the lymphatic channels);
A set of measures is used to diagnose the disease. The dentist examines which reveals the presence of visible symptoms. You will be sent for laboratory tests of blood and urine. Deviations in blood counts: ESR rises to 35-60, a decrease in the number of leukocytes (associated with inflammation), alkaline and acid phosphatase increase, albumins decrease. Urine contains blood cells and proteins. An x-ray confirms the presence of an inflammatory process.
prevent tooth decay
Preventive advice for osteomyelitis of the jaw
A positive outcome in the treatment of osteomyelitis of the jaw is possible with a correct diagnosis and prompt treatment. If the disease is detected in the acute stage – a person recovers in the shortest possible time.There are risks of complications in the form of: symptoms of meningitis, septic shock, pulmonary insufficiency, inflammation of the walls of the veins of the face. 10% of cases ended in death when the sick person ignored the appeal to the doctor. Blood poisoning – main danger.
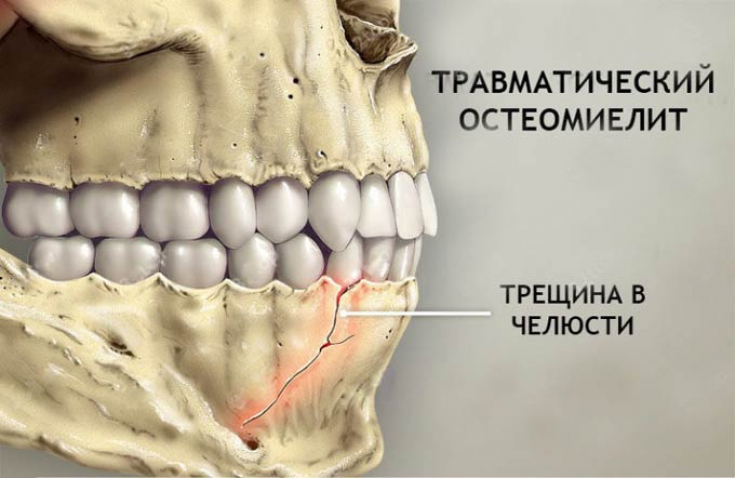 • try to avoid injury to the maxillofacial region – a bruise will create a fissure, and a fissure will create an infection;
• try to avoid injury to the maxillofacial region – a bruise will create a fissure, and a fissure will create an infection;
• do not resort to traditional medicine, the presence of pus – a serious reason to seek medical help;
When treating osteomyelitis of the jaw, the patient will be sent to a hospital, where the first thing to do is to find and remove the cause of the inflammation. Large-scale antibacterial and immunostimulating therapy is being carried out. 
• when the disease is advanced, the jaw is deformed, which leads to discomfort in everyday life;• scarring on the face;
• if the infection spreads to the joints, it will lead to the development of arthritis or arthrosis;
& bull; when a purulent process affects the upper jaw, there is a risk of an abscess of the orbit of the eyeball, and this threatens with loss of vision without the possibility of recovery. development of medicine.
It becomes obvious that
the problems of our teeth
– this is more serious than it seemed before. A timely visit to a doctor increases the chances of a full life in the future.
 Bioceramics in maxillofacial surgery
Bioceramics in maxillofacial surgery
xxxx>
Such a disease as osteomyelitis of the jaw is only gaining fame, even despite the development of medicine.
It becomes obvious that
the problems of our teeth
– this is more serious than it seemed before. A timely visit to a doctor increases the chances of a full life in the future.
Bioceramics in maxillofacial surgery
xxxx>
Such a disease as osteomyelitis of the jaw is only gaining fame, even despite the development of medicine.
It becomes obvious that the problems of our teeth – this is more serious than it seemed before. A timely visit to a doctor increases the chances of a full life in the future.
Bioceramics in maxillofacial surgery
Watch us on YouTube:






Add a comment