Muscular dystonia is a syndrome of damage to the central nervous system, movement disorders characterized by involuntary and irregularly repeated muscle contractions. These contractions cause pretentious stereotyped movements or pathological postures, and the disease itself makes it difficult for patients to adapt socially.
The rarity of the disease is one of the reasons for the difficulties in the diagnosis and treatment of muscular dystonia. The formation of a functional deficit in patients (blindness with blepharospasm, the inability to keep the head in the middle position with spastic torticollis, writing disorders with writing spasm, etc.) makes it difficult for them to socially adapt, leading to early disability.
Classification of muscular dystonia
According to the etiological factor, primary and secondary forms of muscular dystonia (MD) are distinguished.
Primary (idiopathic) is observed in almost 90% of cases and is often hereditary. Currently, the role of a genetic defect in dopamine receptors, anomalies in the structure of proteins involved in neurotransmitter metabolism in the subcortical ganglia are being investigated. The morphological substrate of the disease was not found. The data obtained in the course of neurochemical studies suggest the presence of a neurodynamic defect at the level of the basal ganglia in various forms of MD. oncopathology, etc.
Depending on the prevalence of the pathological process, there are:
focal dystonia (1 anatomical region of the body is involved in the process), including blepharospasm, oromandibular dystonia, spastic torticollis, writing spasm, ambulatory foot spasm, camptokarmia, spastic dysphonia and dysphagia;
- segmental dystonia (2 or more adjacent areas of the body are involved);
- generalized (involving 2 or more non-contiguous areas of the body);
- hemidystonia (involved limbs or whole body according to hemitype);
- multifocal (combining 2 or more focal forms).
- Dystonic movements vary from athetosis to rapid myoclonic twitches, and may change over the course of a day or week. Often they decrease when performing any actions, for example, with spastic torticollis - while playing on the computer, riding a bicycle. Sometimes such paradoxical kinesias cause diagnostic difficulties.
 Diagnosis of muscular dystonia
Diagnosis of muscular dystonia
For all forms of the disease, there are 9 common diagnostic criteria:
presence of dystonic posture;
- dissociation of impaired function of the affected area (for example, with writing spasm, the patient cannot write with a pen, but writes freely with his hand on the board);
- dependence of clinical manifestations on body position and physical activity (aggravated in standing and walking);
- dependence of clinical manifestations on the emotional state;
- use of corrective gestures that reduce the severity of dystonia (for example, patients with spastic torticollis sometimes prevent forced turning of the head by lightly touching the chin with the hand);
- paradoxical kinesias caused by a change in the locomotor stereotype (for example, a patient with dysphonia can sing);
- remissions;
- inversion of functional impairment (for example, the direction of a violent turn of the head with spastic torticollis may change);
- combination of focal forms and their transition from one to another.
- A thorough examination is necessary for all children with dystonia and adults with a generalized form.
Therapy of Movement Disorders
Treatment of patients with focal forms can conditionally be divided into 3 stages.
1st stage. Identification of patients, the appointment of drug therapy (recommended depending on the form of the disease, taking into account concomitant pathology). The duration of the stage is 9–12 months.
In the most common form, spastic torticollis, the following are often prescribed:
benzodiazepines (clonazepam, diazepex, phenazepam); the drug of choice is clonazepam (2 mg tablets). Treatment begins with low doses, gradually increasing them;
- anticholinergics (cyclodol, parkopan, akineton) are used in clonic forms and to enhance the action of clonazepam;
- b-blockers (anaprilin, metoprolol) reduce the clonic component;
- antipsychotics (ORAP, sonapax, eglonil, which do not cause the development of neuroleptic dyskinesias and parkinsonism) are used for clonic forms and low efficiency of other drugs; combination with low doses of reserpine prevents the development of tardive dyskinesia with long-term use of antipsychotics;
- muscle relaxants (baclofen, sirdalud, mylocalm) reduce the tonic component;
- DOPA-containing drugs (Nakom, Madopar) reduce muscle tension in L-dopa-dependent forms with a burdened family history;
- dopamine receptor agonists (bromocriptine, mirapex, ropinirole) can be used in all forms of MD if other groups of drugs are ineffective;
- anticonvulsants (finlepsin, depakine, orfiril, carbamazepine) reduce the severity of pathological muscle tension.
- To reduce the severity of vertebrogenic complications arising from pathological muscle tension, as well as to reduce pain, non-steroidal anti-inflammatory drugs (ibuprofen, diclofenac, meloxicam) are used in medium therapeutic dosages.
In the presence of blepharospasm, the most effective combination of clonazepam with atypical antipsychotics (eglonil, sonapax), and in the combination of blepharospasm with oromandibular dystonia - baclofen.
The role of physiotherapy in the relief of pain and muscular-tonic syndromes is important. It includes magnetic, laser and acupuncture; electrophoresis with magnesium sulfate, sodium oxybutyrate; paraffin, ozocerite applications; exercise therapy is important for patients with spastic torticollis.
2nd stage. It is prescribed when the measures taken are unsuccessful and includes local injections of botulinum toxin. In neurological practice, the drug has been used since the late 1980s. Botulinum toxin is a potent nerve poison that, when injected intramuscularly or subcutaneously, causes chemical denervation of the muscles, and when locally injected into the muscle, causes partial paresis, but does not impair its ability to voluntary contractions.
Botulinum toxin is most effective when a small group of muscles is involved in the pathological process, ineffective in writing spasm, ineffective in generalized muscular dystonia. The method is the therapy of choice in the treatment of focal forms of muscular dystonia (spastic torticollis, blepharospasm), as well as facial hemispasm.
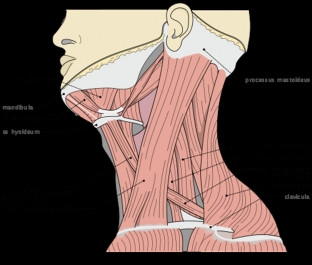
Injections of the drug are prescribed in the presence of medical indications, severe forms of the disease and the ineffectiveness of drug treatment during the year. Before the introduction of botulinum toxin, during examination, palpation or using EMG, the muscles most actively involved in dystonic spasm are identified.
Absolute contraindications to the introduction of botulinum toxin are pregnancy, breastfeeding, certain neurological diseases (myasthenia gravis, Lambert-Eaton syndrome, amyotrophic lateral sclerosis), severe somatic pathology in the stage of decompensation;
relative contraindications - acute infectious diseases, inflammatory processes at the intended injection points, taking antibiotics from the aminoglycoside group.
After the injection, the risk of adverse reactions is low, moreover, they are transient (pain, hematomas, paresis may be observed at the injection site, dysphagia and dysarthria when the drug is injected into the neck area, and ptosis in the treatment of blepharospasm). Systemic side effects, such as muscle weakness away from the injection site, are extremely rare.
This method compares favorably with the rest - drug and non-drug: the clinical effect is achieved in 85-90% of cases and lasts 2-3 months (fixed and longer remissions with less pronounced relapse in the future). As a rule, patients need repeated injections of the botulinum toxin preparation: with spastic torticollis - 2 injections per year, with blepharospasm - 3-4.
3rd stage. The period of weakening of the action of the botulinum toxin preparation. To prolong the effect, drug therapy of the 1st stage is used - with an individual selection of physiotherapy treatment and doses of drugs.
Surgical treatment is used depending on the form of dystonia at the muscular, neural, radicular or cerebral levels. However, the therapeutic effect is often transient or associated with dangerous or maladaptive functional disorders (speech, paresis, instability of the spinal segments). Therefore, in recent years, surgical methods have been resorted to less and less.
Modern diagnostics and correctly chosen tactics for the treatment of focal muscular dystonia can significantly reduce the period of temporary disability, reduce disability and the number of hospitalizations in neurological hospitals, increase social activity and quality of life of patients.
According to medvestnik.by






Add a comment