Urticaria — a heterogeneous group of diseases characterized by diffuse or limited rash in the form of blisters or papules, which are accompanied by itching.
Chronic urticaria (HC) characterized by recurrent episodes, that occur at least two once a week for 6 weeks.
Understanding the clinical manifestations associated with chronic urticaria and its subtypes improves diagnosis and facilitates a personalized approach to treatment.
That is why the purpose of this article on estet-portal.com is to highlight the approach to patient management with chronic urticaria based on the provision of evidence-based recommendations to clarify the diagnosis and develop treatment strategies.
- Classification and pathogenesis of chronic urticaria
- International Guidelines for Determining the Causative Factor in Patients with Chronic Urticaria
- Difference diagnosis in patients with chronic urticariath
Classification and pathogenesis of chronic urticaria
Chronic urticaria (HC) can be divided into the following forms:
- spontaneous or idiopathic - characterized by the sudden onset of symptoms, the cause of which remains unknown;
- inducible - occurs under the influence of certain factors.
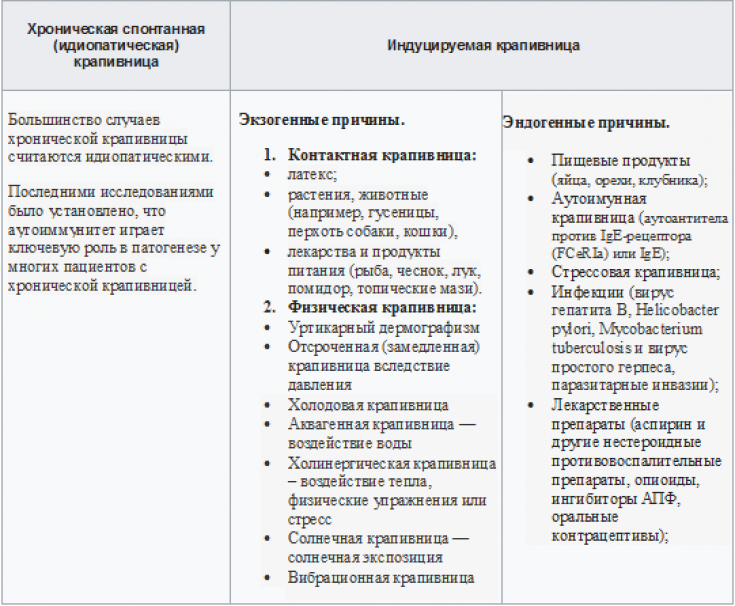
It has also been reported that two or more forms of chronic urticaria coexist in the same patient.
Follow us on Instagram!
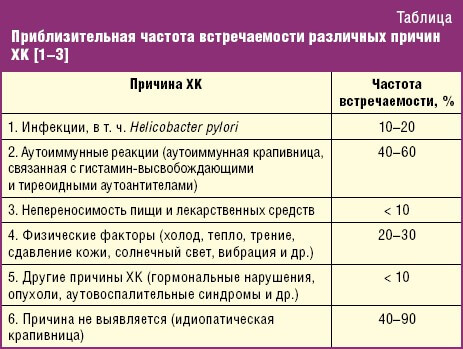
The pathogenesis of chronic urticaria is not fully understood. Mast cells, basophils, histamine and other mediators play a key role.

"Common Pathway" for spontaneous and induced urticaria − the release of histamine and other pro-inflammatory mediators, which explains the effectiveness of H1-blockers as first-line therapy.
Specific conditions in dermatology that are accompanied by skin itching
Primary causes of neurotransmitter release are not fully understood and are likely to differ.
Possible factors that lead to degranulation of mast cells or basophils are poorly understood and likely to differ between physically induced urticaria and urticaria secondary to autoimmune disorders

Tests to determine the etiological factor, depending on the history, include the following recommendations.
1. International recommendations:
- detection of infections (e.g. Helicobacter pylori);
- detection of type I allergy (spectrum of allergens);
- functional antibodies (for example, to gliadin, thyroperoxidase);
- thyroid hormones and autoantibodies;
- tryptase as an indicator of systemic allergic inflammation;
- skin tests for type 1 and 4 hypersensitivity (prick and patch tests);
- exclusion of pseudo-allergens from the diet for 3 weeks.
All the dermatologist needs to know about topical glucocorticoids
2. US Standards:
- limited lab testing;
- routine tests rarely show clinically significant abnormalities
- Differential diagnosis in patients with chronic urticaria
International recommendations:
1. If an autoinflammatory disease is suspected, the following tests should be performed
: erythrocyte sedimentation rate (ESR) and/or C-reactive protein;
- test for paraproteinemia (in adults);
- Screening for neutrophil-rich infiltrates in skin biopsy;
- detection of gene mutations.
- 2.If congenital angioedema is suspected
Complement C4;
- C1 inhibitor level and function;
- antibodies to C1q and C1 inhibitor;
- detection of gene mutations.
4.If the duration of the rash> 24h
− biopsy to determine the presence of vasculitis (vascular damage in the papillary and reticular dermis and/or fibrinoid deposits in the perivascular or interstitium).Ways to overcome toxic skin reactions in the practice of a dermatologist. (Part 1)
Today, the pathogenesis of
chronic urticaria is not fully understood, andsteps in diagnosis and treatment need to be improved, possibly with wider use in clinical practice a dermatologist together with an allergist of the latest arsenal of immunobiological agents based on monoclonal antibodies. Follow our news and stay up to date with the latest discoveries in medicine!
Modern approaches to the diagnosis and treatment of vitiligo







Add a comment