In recent years, the problem of toxic skin reactions has become apparent in the practice of a dermatologist, which reflects some unexpected aspects of modern medicine and, oddly enough, is associated with the rapid development of pharmaceutical areas.
Continuous improvement of medical directions has allowed to cope with serious illnesses, to move to clinical protocols based on evidence-based medicine. But the skin – it is also an important organ of the excretory system, so all toxic skin reactions reflect internal processes in the body.
Learn in the article on estet-portal.com about the main mechanisms of toxic skin reactions in the practice of a dermatologist.
Causes of toxic skin reactions
The last decades are characterized by a large-scale development of pharmacological directions, hundreds of medicines have appeared that allow treating serious diseases. In particular, the emergence of new drugs in dermatology has become a revolution in the treatment of severe chronic dermatoses.
Follow us on Instagram!
The fact that these drugs go through a complex path of multi-stage, multi-center studies gives confidence to a dermatologist. However, a number of unexpected difficulties are encountered in a convincing and flawless way of implementing these tools.
What a dermatologist should know about hives in children
Recently, cases of lack of alertness regarding possible individual intolerance to medicines have become more frequent, self-medication has reached a large scale (through advertising of drugs on social networks and the false "non-European" practice of over-the-counter sales) and attachment to unjustified polypharmacy. These aspects of progress in medical science, of course, have caused unpleasant complications in the form of drug-induced toxic skin reactions.
Toxic skin reactions in the practice of a dermatologist
Along with the manifestations of internal organs and systems, the number of toxic skin reactions of varying severity has noticeably increased. The skin is the most common target for drug-induced reactions. Most toxic skin reactions (approximately 90%) are related to drug hypersensitivity. Drug-induced rashes are predominantly caused by systemic drugs. Most drugs can induce erythematous rashes in up to 1% of people who take them.
It is toxic skin reactions that make the dermatologist pay attention to a rather new problem and look for ways to prevent and treat these skin reactions.
Clinical picture of toxic skin reactions
The clinical picture of drug-induced toxic skin reactions is varied. So, in 1-3% of patients taking drugs, there is a transient benign erythema that occurs on the 6-9th day after taking the drug, and one in 10 thousand patients develop severe toxic skin reactions. It is often difficult to establish a diagnosis of toxic skin lesions.
Main risk factors for melanoma
However, it is this guess about the individual reaction to the drug that helps the dermatologist to establish a diagnosis, exclude the causative drug and, in some cases, save the patient's life. It is important for a dermatologist during a diagnostic search to establish the category of severity of skin reactions, to distinguish the type of skin reaction, and even to determine a possible prognosis of mortality.
Classification of toxic skin reactions
According to the modern classification, the following clinical variants of toxic skin reactions are distinguished:
1. Skin Adverse Reactions (SCAR),
2. bullous fixed drug-induced rashes (BFDE),
3. acute generalized eczematous pustulosis (AGEP),
4. drug reactions with eosinophilia and systemic symptoms (DRESS syndrome),
5. Stevens-Johnson Syndrome (SJS),
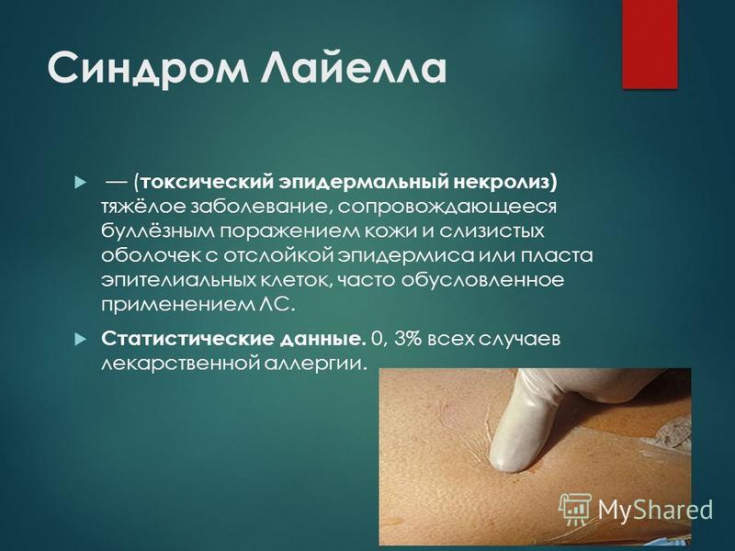
6. toxic epidermal necrolysis (TEN).
Some forms of toxic skin reactions are so severe that they can be fatal, even regardless of the measures taken.
Thus, it has been established that the comparative assessment of the mortality prognosis is: with FDE - 0%, with AGEP - 5%, with DRESS - 10%; at SJS / TEN - 25% (highest danger).
A new antibiotic in the treatment of pyoderma
Groups of drugs that cause toxic skin reactions
Screening evaluations of many groups of drugs are currently underway, which has revealed a fairly high level of skin reactions to drugs, which is generally 0.1-1% among treated patients. Aminopenicillin, sulfonamides, anticonvulsants, non-steroidal anti-inflammatory drugs (NSAIDs) and ACE inhibitors have been found to be the leaders in this rating of causes of toxic skin reactions.
In general, medicines are specific to each individual case. According to statistics, only 1 million people suffer annually from the side effects of the use of medicines in the world (in 180 thousand cases − death).
Methods for preventing atopic dermatitis in children
Medical toxic skin reactions in pediatric practice are of particular concern in the practice of a dermatologist. It has been shown that the most popular drugs prescribed to children on an outpatient basis are antibiotics (74% of patients), antihistamines (74%), immunotherapy (52%), vitamins (42%), nootropics (39%), probiotics ( 30%), NSAIDs (22%), uroseptics (17%), sorbents (13%), mucolytics (12%). The clinic of skin rashes is diverse and has its own characteristics in terms of the rate of occurrence and, most importantly, severity.
Therapeutic efficacy of histamine blockers in eczema
The following approaches to overcoming toxic drug-induced skin reactions can be distinguished: the exclusion of polypharmacy, the timely diagnosis of toxic drug-induced skin reactions, the appointment of hepatoprotectors, the exclusion of systemic drugs by replacing them with topical ones.
Immune function of the skin on guard of the health and order of the body







Add a comment