Bacterial infections of the skin and soft tissues – one of the most severe comorbidities in the ICU. A well-chosen treatment regimen in such cases can save the life of patients. Unfortunately, one of the modern problems of this category of pathologies – it is antibiotic resistance.
Find out in the article on estet-portal.com what algorithm for diagnosing and approaches to antibiotic therapy of skin and soft tissue infections should a dermatologist use to keep the patient healthy.
The most common pathogens of skin and soft tissue infections
Older age, diabetes mellitus, obesity, malignancies, cirrhosis of the liver, and long stays in the intensive care unit − risk factors for skin and soft tissue infections.
Follow us on Instagram!
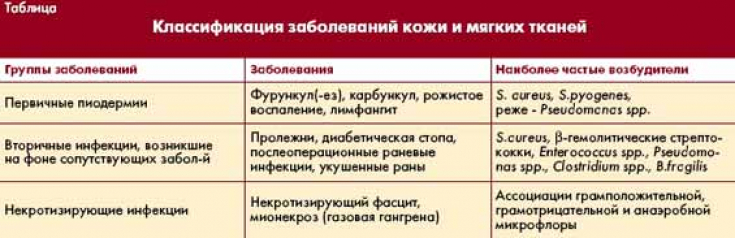
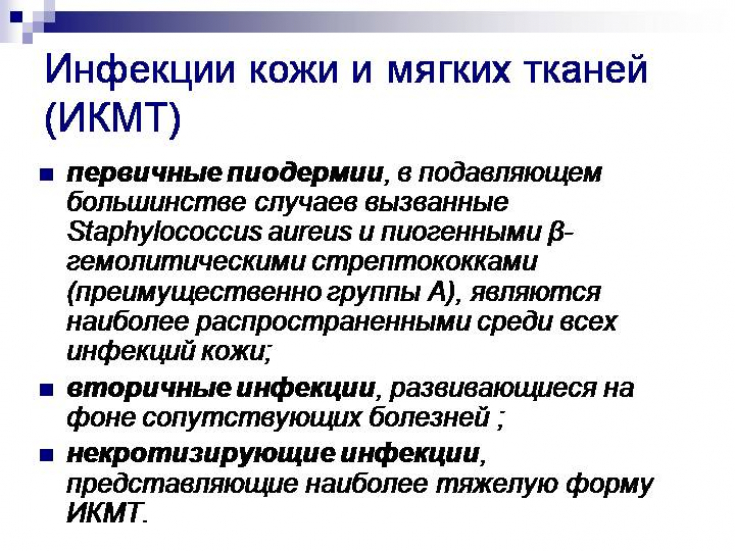
Gram-positive organisms (Staphylococcus aureus) − most common organisms responsible for skin and soft tissue infections. E. coli and Pseudomonas .minus; frequent pathogens among gram-negative microorganisms.
Five skin manifestations that can save lives if diagnosed
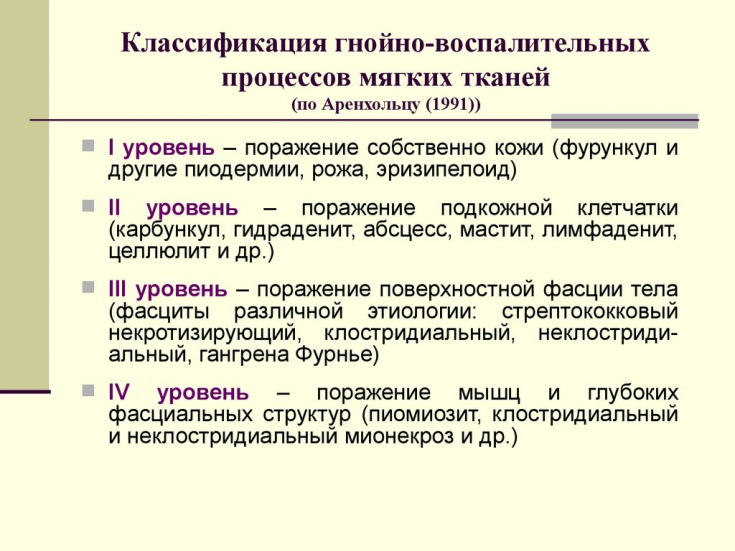
MRSA (Methicillin-resistant Staphylococcus aureus − methicillin-resistant Staphylococcus aureus) and Gram-negative organisms producing ESBL (Extended-spectrum beta-lactamase − extended-spectrum beta-lactamase) are the most common causes of skin and soft tissue infections in the ICU therapy. Monomicrobial necrotizing fasciitis is most commonly caused by Streptococcus pyogenes; mixed coliforms, anaerobes and staphylococci are the most common causes of polymicrobial necrotizing fasciitis.
Approaches of a dermatologist to antibiotic therapy of skin and soft tissue infections
Vancomycin, teicoplanin, daptomycin, and linezolid are effective in skin and soft tissue infections caused by MRSA. Piperacillin-tazobactam and carbapenems are most effective in ESBL produced by Gram-negative organisms. Penicillin, clindamycin are the most effective as part of antibiotic therapy for monomicrobial necrotizing fasciitis, while the combination of piperacillin-tazobactam, fluoroquinolone and clindamycin is effective for polymicrobial fasciitis.
For non-suppurative infections of the skin and soft tissues of moderate severity, the introduction of penicillin or clindamycin as a first-line antibiotic is recommended. Severe non-suppurative skin and soft tissue infections should be treated with piperacillin-tazobactam plus an anti-MRSA drug (vancomycin, teicoplanin, daptomycin, or linezolid).
In addition to the constant work and supervision of a dermatologist with this group of patients, an accompanying surgical examination or wound debridement is necessary in case of severe non-purulent infections of the skin and soft tissues.
For severe purulent skin and soft tissue infections, incision and drainage of the wound with empiric antibiotic therapy, which includes piperacillin-tazobactam plus an anti-MRSA drug (vancomycin, teicoplanin, daptomycin, or linezolid), is recommended.
All the dermatologist needs to know about topical glucocorticoids
Duration of antibiotic therapy for skin and soft tissue infections
A short course of antibiotic therapy is adequate for uncomplicated skin and soft tissue infections, while complicated infections require a long course of antibiotic therapy.
Severe non-suppurative skin and soft tissue infections should be treated for at least 5 days with antibiotics. Severe skin and soft tissue infections with organ dysfunction should be treated with a prolonged course of antibiotics for 2-3 weeks.
Empirical dual-class (with different mechanisms of action) combination antimicrobial therapy for skin infections of unknown etiology in the intensive care unit is associated with better clinical outcomes. Empiric antibiotic therapy with piperacillin-tazobactam or carbapenems in combination with aminoglycosides or a fluoroquinolone showed adequate broad antimicrobial activity and improved clinical outcomes compared with monotherapy.
Toxicoderma: causes, symptoms, diagnosis, treatment
Empirical antibiotic therapy should attempt to provide antimicrobial activity against the most likely pathogens based on clinical signs and local patterns of microorganism susceptibility and resistance. A competent approach by a dermatologist, surgeon and resuscitator can save a patient's life in some of the most difficult situations in the intensive care unit.
Insidious toxicoderma: the main clinical forms of the disease







Add a comment