Readers estet-portal.com offers a description of a special surgical technique based on the movement of facial tissues and platysma fibers to the places where they are in young people. Studies regarding this procedure were carried out on 305 patients (85% women) over the past 3.5 years. Patients differed in age - from 41 to 75 years (mean 54 years).
The minimum period of postoperative observation for all patients was 6 months, for 60% of them this period was extended to 2.5 years. During the same procedure, temporal lift and facelift were performed for 262 patients, and blepharoplasty for 278 patients. In 95% of cases, local anesthesia and sedatives were used under the supervision of an anesthesiologist.
We present you an interview with Alan Fogli,
- Professor of the International Association of Aesthetic Plastic Surgeons ISAPS;
- Honorary President of the National Organization for Plastic, Reconstructive and Aesthetic Surgery;
- Member of the French Association of Plastic, Reconstructive and Aesthetic Surgeons;
- Member of the Argentine Association (Buenos Aires) for Plastic, Reconstructive and Aesthetic Surgery;
- Founder of CliniquedechirurgieesthetiquedudocteurFogliAlain, Marseille (France).
Preoperative marking for correction of the face and platysma muscles
First, the damage to the skin that needs to be healed has been studied. Before the operation, marking is carried out on patients in a sitting position. We identify the first lesion to be treated, examine zygomatic fat ptosis, cheeks, vertical wrinkles from the corners of the lips to the chin, nasolabial folds and platysma bands. We then label the anchor structures.
Marking is applied at the level of the cheekbones and the fibrous tissue located between the subcutaneous auricular junction and Lauré's fascia anterior to the earlobe. The line drawn between these two points roughly reflects the anterior margin of the parotid aponeurosis. The fibers of the anterior and posterior edges are noted after voluntary contraction of the platysma muscle. Marking is carried out at a distance of 4 - 4.5 cm vertically above the prelobar fibrous tissue. The direction vectors are similar to those used by Tonerd and Verpel in their minimal access cranial suspension technique (Fig. 5a).
They go from the previously described prelobar fibrous tissue, then through the cheeks and submental bands of platysma to the anterior edge of the parotid aponeurosis and from the anterior zygomatic fat pack to the base of the zygomatic bone. At the end the markings necessary to separate the skin and reach the pre-zygomatic fat and platysma fibers are carried out (Fig. 5b).

Fig. 5. (a) Various vectors: (1) between platysmal fibers and prelobar fibrous tissue, including ear platysmal ligaments and Lore's fascia; (2) between pretemporal fatty layer and periosteum of the cheekbone; (3) between the SMAS and the anterior face of the parotid fascia. (b) Passage of the needle between the platysma fibers and the prelobar fibrous tissue and its return into the fibrous tissue. (c) Attachment of the platysma and prelobar fibrous tissues, indicating the oval and angle between the neck and chin. (d) Attachment of the pretemporal fat to the zygomatic bone and continuous suture between the SMAS and the anterior facet of the parotid fascia from the zygoma to the prelobar fibrous tissue. (e) Continuous seam completed. Restitution of correction of the temporal contour of the nasolabial folds was performed. Marking and incision of the skin for correction of the face and platysma muscles
The markings for skin incisions are made under the sideburns, slightly lower for men depending on the length of the sideburns. Next, the line is attached to the root of the ear helix to record the natural distance of the hairless skin between the tank (Fig. 5b) and the auricle. It passes at a distance of 1 mm in front of the posterior edge of the tragus. Then, in front of the earlobe, it rises parallel to the line behind the ear and is carried forward a few millimeters towards the auricle until it reaches a certain level, passing through the root of the spiral. The marking line then curves and follows the hair implantation line for about 2 cm before changing direction by 90° becoming intracapillary and following the horizontal line for more than 2 cm.
Surgical technique for facial correction and platysma
Infiltration
. This technique is used in sedated patients using local anesthesia with xylocaine 0.5% and epinephrine (1.5 mg per 160 ml for both sides). A 25 G needle is used for incision areas.Intervention
. This is a surgical cut of the skin that begins with a #15 scalpel and continues with curved blunt-tipped scissors following a pre-marked pattern. Hemostasis is carried out carefully.The Vicryl stitch is made from top to bottom with a bent needle and captures the prelobar fibrous tissue. You need to make sure that the ear cartilage does not move and the attachment is strong. Then the needle itself captures the posterior fibers of the platysma muscle according to the preoperative marks that were made during the separation of the skin. The effect of bringing the platysma muscle into a tense state should be evaluated. The angle between the chin and the neck must be marked and the entire neck must be covered. If the effect is insignificant, you must try again.
When the platysma fibers are anchored, a new level of these fibers is covered at the level of the mandible. A high tension stitch is applied to this site with elevation of the muscle, and the skin joins the prelobar fibrous tissue here (Fig. 5c and d). This movement of the platysma, in which the skin remains attached and forms voluminous folds like excess skin, will be removed after the submucosal aponeurotic system (SMAS) is anchored at the level of the face. Using Vicryl 2\0, pick up and raise the pre-zygomatic fat layer, then suture the periosteum of the cheekbone with an inverted stitch. We cut a short thread and lay a long suture between the submucosal aponeurotic system (SMAS) & nbsp; and the anterior face of the parotid aponeurosis from the periosteum of the cheekbone to the prelobar fibrous tissue (Fig. 5 eif). This suture should be applied carefully and should not leave any roughness, and on the surface the sutures will be visible through the skin for several months. 4 to 5 final passes of the seam reduce the tension of the previous seam.The cheek contour is adjusted with the back of the scissors along the seam. The haemostasis is checked again. Elevation of the pre-zygomatic fat and SMAS allows for a harmonious distribution of volumes and achievement of the Augi curve.
Then, the skin flap is pulled back in the direction of the posterior vector of the facial area (Fig. 6a). This maneuver should not create folds at the level of the zygomatic area, which can be eliminated in the same operation with a special technique. At the behind-the-ear level, the skin overlay vectors should be as far back as possible without touching the hairline.
The key sutures under and above the tragus, behind the ears, and the hairline sutures are applied without tension (Fig. 6b). The flaps are attached after degreasing and thinning of the skin covering the tragus. But before that, you need to make sure that there is a slight weakening in front of it, which will provide a perfectly natural tragus.
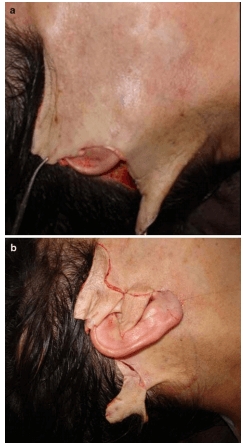 Fig. 6. (a) Excess skin to cover with posterior and horizontal vector without any tension. (
Fig. 6. (a) Excess skin to cover with posterior and horizontal vector without any tension. (
b) Key seams on top and bottom of tragus. Creating Adjusted Flaps An intradermal suture is then applied with 2 \ 0 propylene. Only at the end of the operation, when all the volumes have been transferred, does it need to be assessed for the need for fat implantation.
Details of a special technique for correcting age-related changes in the area of platysma and some structures that allow keeping facial muscles in a taut state will be personally presented at the ISAPS World Congress, which will be held in Kyiv on May 19-20,In the following article, readers of estet-portal.com are offered a description of the technique (SPMA)
for fixing the skin and muscle of platysma, developed by Alan Fogli
, as well as and some results of this technique in elderly patients.







Add a comment