Obesity is one of the most complex medical and social problems of our time. In recent years, in many countries of the world, the incidence of obesity has increased tenfold, and the actual prevalence in most European countries today is about 20%.
Therefore, the ESE has issued updated recommendations for management of patients with obesity and endocrine pathology, which are presented in this article on estet-portal.com
- Diagnosis and search for causes of obesity
- Thyroid dysfunction as a cause of obesity
- Hypercortisolism as a cause of obesityia
Diagnosis and search for causes of obesity
Body weight alone is not a sufficient guideline for diagnosis. It is also necessary to focus on body mass index (BMI) and waist to hip ratio.
Follow us on Instagram!
While a simple definition of BMI is likely a simplistic approach to diagnosing obesity, however, BMI is easily calculated and there is no data yet to show that sophisticated diagnostic methods are of great advantage in establishing a diagnosis of obesity.
Effective diet in the management of the patient with metabolic syndrome
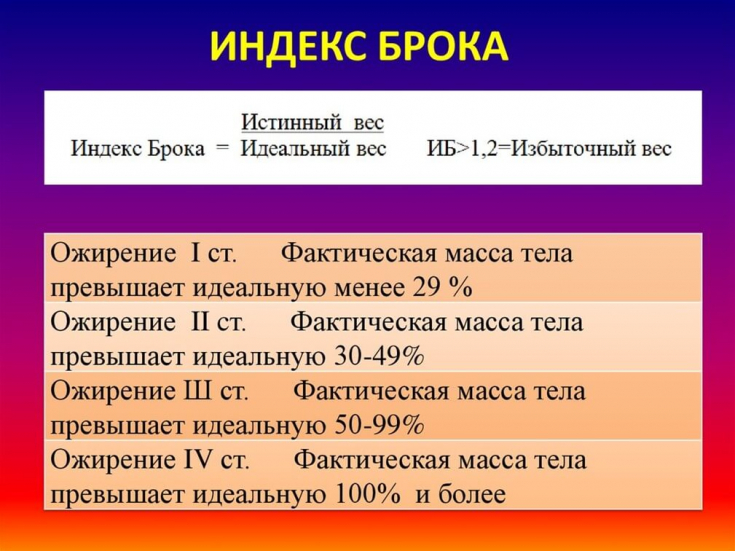
Increased BMI leads to a series of hormonal changes. In addition, with obesity, there are concomitant endocrine diseases that need proper diagnosis and treatment.
ESE (European Society of Endocrinology) has developed guidelines for the management of obese patients. The purpose of the settings is to provide clinicians with practical guidance on therapeutic care for obese patients.
It is suggested that all patients measure body weight and height to determine BMI. For the routine diagnosis of obesity, it is sufficient to determine BMI> 30 kg / m2. Waist measurement is also recommended as an additional diagnostic test, especially if BMI
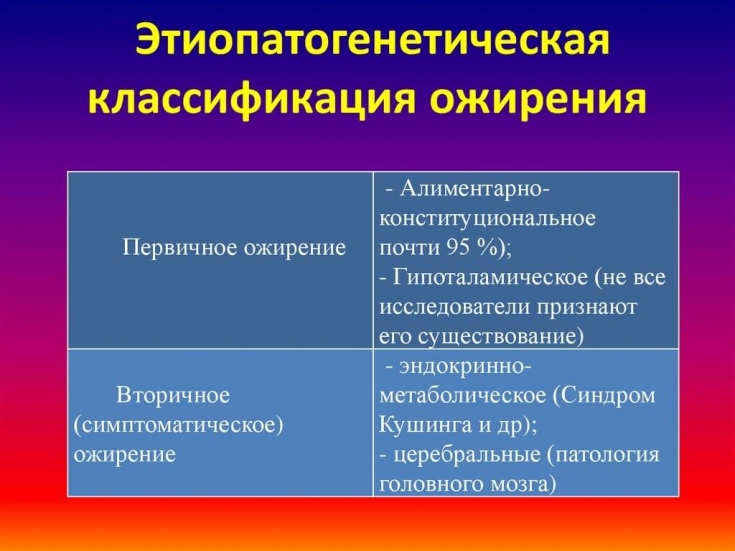
Also, for the diagnosis of obesity, the calculation of Brock's index.
It is important to consider that all prescribed medications and dietary supplements can affect the concentration ofhormones.
Thyroid dysfunction as a cause of obesity
Thyroid function is usually assessed regardless of the cause of obesity, as hypothyroidism is one of the most common endocrine diseases in the world. In Europe, the prevalence of hypothyroidism ranges from 0.2-5.3%, and the prevalence of undiagnosed hypothyroidism is estimated to be around 5%.
Symptoms of hypothyroidism are non-specific and can be perceived as symptoms of obesity, namely:
- fatigue;
- depression;
- convulsions;
- menstrual irregularities;
- weight gain.
Also, it has been statistically shown that a high prevalence of hypothyroidism occurs precisely in the presence of obesity.
Because hypothyroidism is quite common in the population and can exacerbate weight gain as well as worsening comorbidities in obesity, monitoring of thyroid function.
Drug therapy for diabetic complications
It is recommended that the diagnosis of hypothyroidism be based on the level of thyroid stimulating hormone (TSH). If the TSH level is elevated, it is recommended to test for free thyroxine (T4) and anti-thyroid peroxidase (anti-TPO) antibodies.
According to American guidelines, TSH is the best screening test for thyroid dysfunction in most clinical situations in which a normal TSH level is sufficient to rule out primary hypothyroidism.
Central hypothyroidism with low TSH and disproportionately low T4 is uncommon − 1% of cases of hypothyroidism. Therefore, the determination of T4 should be carried out only in the case of an elevated level of TSH.
The most common cause of hypothyroidism is chronic autoimmune thyroiditis. Elevated concentrations of thyroid antibodies are found in 11% of the general population. Thyroid antibody profiles are recommended to diagnose autoimmune hypothyroidism and to identify patients who may develop secondary hypothyroidism in the future.
Sirtuins – longevity proteins for rejuvenation of the skin and the body as a whole
Thyroid hormone preparations and their derivatives have been widely used in the last century as drugs for the treatment of obesity. However, this therapeutic tactic is outdated, since insufficient effect of thyroid hormones on weight loss has been found and development of iatrogenic thyrotoxicofor.
Hypercortisolism as a cause of obesity
Obesity is usually a comorbid condition in most of the so-called pseudo-Cushing syndromes (pseudo-Cushing state). In the presence of central obesity, which is accompanied by specific signs and concomitant cardiovascular risk factors (AH, DM 2), the diagnosis of "Cushing's syndrome" should be excluded; (SK).
There is also evidence that subclinical MC is more likely to be the cause of obesity. Therefore, the ESE Working Group recommends screening for hypercoticism in patients who, in addition to obesity, have other specific symptoms of hypercoticism.
Such signs include:
- skin atrophy;
- osteoporosis;
- spontaneous ecchymosis;
- proximal myopathy;
- stretch marks.
Other features are common to both MC and obesity such as:
- central obesity;
- type 2 diabetes;
- arterial hypertension;
- depression.
If hypercortisolism is clinically suspected, a biochemical blood test.
More interesting information on our YouTube channel:







Add a comment